 |
History
A 33-year-old white female presented with a chief complaint of blurry vision in both eyes, more so in the left than the right, for the previous three months. She was able to pinpoint that the constant blur developed just after she was in an auto accident. She reported hitting the left side of her head on the back of the passenger seat, in a slow moving vehicle accident while not wearing a seat belt. Her previous ocular and systemic histories were unremarkable and she denied any known allergies to medications or other substances.
Diagnostic Data
Her best corrected entering Snellen visual acuity was 20/20 in the right eye and 20/30 in the left eye at distance and near. Refraction revealed hyperopia of +0.75D in the right eye and +1.50D in the left eye, with no improvement in vision for either eye. The pertinent biomicroscopic findings are illustrated in the photographs. Her intraocular pressure was measured as 15mm Hg in the right eye and 18mm Hg in the left eye using Goldmann applanation tonometry. Dilated fundus examination revealed no significant posterior pole or peripheral retinal findings. The nerves were distinct, with cup-to-disc ratios of 0.3/0.35 in both eyes.
An optical coherence tomography scan was performed and revealed no sign of macular edema, hole, sustained vitreomacular traction or retinal detachment in either eye. Laser interferometry was performed, with improved visual acuity measuring 20/25.
Your Diagnosis
What is your diagnosis and presumed cause of the condition? How would you approach this case? What is the likely prognosis?
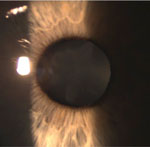 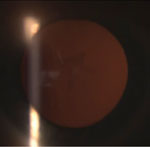 | |
| Slit lamp images of a 33-year-old white female who presented with a chief complaint of blurry vision in both eyes, but more so in the left eye. |
Discussion
The diagnosis in this issue is rosette cataract secondary to the blunt trauma to her eye sustained as a result of the auto accident. Trauma remains the leading cause of monocular blindness in patients 45-years-old or younger.1-4 Males are affected four times more than females. Clinical findings may present as a result of acute, sub-acute, or longstanding sequelae.1-4
Acute traumatic cataracts, also known as stellate or rosette cataracts, result from anterior or posterior subcapsular lenticular changes induced by mechanical blunt or penetrating trauma.1-3 They may be stable or progressive and occur due to shearing forces that introduce pathologic changes to lenticular composition.1,4,5
Courville et al introduced the concept of coup (direct force injury) and contracoup (opposite the direct force) to the category of traumatic injury.1-3,6 Contracoup injury is based upon secondary shockwaves that transverse the location and axis of impact.1-3,6 Resulting contralateral expansion of the lens induces tissue remodeling and accelerated opacification.1-6 This mechanism is responsible for the stellate shape of rosette cataract formation.1,2,5,6 As the impact occurs, an anterior compression along the axis of impact produces forces which cause posterior expansion leading to rupture of lens fibers with disorganization.5-7 Specifically, the lens capsule, lenticular zonules or a combination can be affected depending on severity of trauma.1,2,7,8 In cases involving penetrating injuries, the size of the rent determines the degree of opacification. Large lenticular penetrating injuries can cause rapid lenticular hydration that can lead to complete lens opacification.1-3
On a biochemical level, when trauma to the lens occurs, disruption of adenosine triphosphate (ATP)-dependent sodium/potassium (Na+/K+) ion pumps causes osmotic hydration to occur.2,9 Influx of sodium ions and water pour into affected lenticular substrates producing excessive swelling of lenticular epithelial cells.2,9 Initially, this influx of fluid causes thickening of anterior and posterior cortical lens fibers.2 Over time, reduction of swelling leads to proteolysis, aggregation and lenticular cell conformation resulting in radial whitening and the typical “flower-shape” appearance of the lens.1,2,9
Treatment
Rosette cataracts may disappear, remain stationary, or progress to total lens opacification.2,10 Treatment depends on the location of the cataract in relationship with the visual axis.1,8-11 Prognosis is not only based on the severity of injury itself, but also in concert with the significance of adjacent associated ocular injury and whether or not the injury involved an open or closed globe.1,7-11 Glaucoma, ocular inflammation, macular edema, retinal detachment and macular hole formation are co-morbidities.1,6-11
Standard phacoemulsification can be performed when normal lens capsule integrity and sufficient zonular support is present.1,8-11 When the stability of the lenticular zonules is absent or if the capsule has sustained a rupture or if a concurrent systemic pathology such as Marfan’s syndrome, homocystinuria, or pseudoexfoliation syndrome is present, raising additional issues with standard techniques for removal, the strategy must be altered.1-3,10 Pars plana lensectomy with or without limited vitrectomy is another option.1,8-11 At the time of injury hyphema, inflammation, and vitreous hemorrhages can occur; further chronic inflammation can lead to the development of posterior or peripheral anterior synechia, making surgical intervention difficult to perform.1,8-11 While visual gain post traumatic anterior segment surgery is a complex process, studies also suggest that surgical intervention yields statistically favorable visual acuity even following open globe injuries.10,11
The patient was educated about treatment options for proper removal of the rosette cataract. She was referred to a surgeon for extraction resulting in 20/20 uncorrected Snellen acuity in both eyes.
Dr. Andrew Gurwood thanks Dr. Christopher T. Luft for contributing this case.
1. Kumar A, Kumar V, Dapling RB. Traumatic Cataract and Intralenticular Foreign Body. Clin Experiment Ophthalmol. 2005;33(6): 660-1.2. Wevill M. Basic Science of the Lens. In: Yanoff M, Duker JS. Ophthalmology, 3rd Ed. Edinburgh, Mosby Elsevier; 2009: 504-7.
3. Shah, M A, Shah S M, Shah S B, et al. Morphology of Traumatic Cataract: Does it Play a Role in Final Visual Outcome? Brit Med J. Open. 2011;1(1): 3-6e.
4. Luntz MH. Clinical Types of Cataract. In: Tasman W, Jaeger E. Duane’s Clinical Ophthalmology Philadelphia: Lippincott;1998: 13-14.
5. Kuhn F, Dante JP. Ocular Trauma: Principles and Practice. In: Gumpert E, Kurup V. 1st Ed. New York, Thieme. 2002; 181-200.
6. Courville CB: Forensic Neuropathology. J Forensic Science 1962;7(1): 100-102.
7. Wolter JR. Coup-contrecoup Mechanism of Ocular Injuries. Am J of Ophthalmol. 1963; 56 (11):785-796.
8. Delori FO, Pomerantzeff O, Cox MS: Deformation of the Globe under High-Speed Impact: its Relation to Contusion Injuries. Investigative Ophthalmol and Vis Sci. 1969;8(2): 290-301.
9 Boorstein J M, Titelbaum D S, Patel Y, et al. CT Diagnosis of Unsuspected Traumatic Cataracts in Patients with Complicated Eye Injuries: Significance of Attenuation Value of the Lens. Am J of Roentgenology. 1995;164(1): 181-84.
10 Shah, M, Shah S, Prasad V, et al. Visual recovery and predictors of visual prognosis after managing traumatic cataracts in 555 patients. Indian J of Ophthalmol. 2011; 59(3):217–222.
11. Shah, M, Shah S, Prasad V, et al. Comparative Study of Final Visual Outcome between Open- and Closed-globe Injuries following Surgical Treatment of Traumatic Cataract. Graefe's Archive for Clinical and Experimental Ophthalmol. 2011;249(12): 1775-1781.

