Clinicians today use more sophisticated technologies than ever before to manage patients through the onset and progression of glaucoma. While these technologies help us manage a patient’s intraocular pressure (IOP) and other factors, optometrists must keep the patient’s comfort, happiness and quality of life in mind when creating a treatment plan.
Traditionally, eye doctors would suggest glaucoma treatment begin when a patient’s IOP measures 21mm Hg. However, researchers now believe that determining when to treat requires a multifaceted approach that uses a complex array of factors.1 But, perhaps the time to start treating can’t be based on numbers alone. In fact, the patient’s ability to function visually day to day may be just as integral as any diagnostic measurement.
This article reviews the impact glaucoma has on our patient’s lives and the measures we can take to help prevent it from robbing them of their independence.
 | |
| Glaucoma’s effect on peripheral visual acuity can leave many patients feeling anxious or apprehensive about driving. Stock Images: ©iStock.com/JobsonHealthcare. |
Perception
Patient perception of quality of life depends on the severity of the disease—some patients with severe vision loss have indicated a willingness to trade years of their lives for better vision. A study comparing the responses of 228 patients with glaucoma to 12 blind patients and 12 controls with normal vision found 45 (20%) glaucoma patients were willing to trade time for improved vision, compared with six (50%) blind patients.2 Glaucoma patients with counting fingers or worse vision in their better eye also indicated more willingness to trade time or risk death (i.e., standard gamble method) for better vision, compared with patients with 20/20 or 20/25 in their better eye.3 Patients with more severe binocular visual field loss also reported feeling less confident and more anxious during certain daily activities, such as crossing the street.4
Autonomy
Difficulty with reading is one of the most frequent complaints among people with glaucoma, and the most common cause for low vision referrals.4 On average, those with advanced bilateral visual field loss have been shown to read an average of 29 words per minute slower and are twice as likely to make a mistake than those without glaucoma.5 Silent reading skills are especially affected: patients with glaucoma exhibited a 16% decline in silent reading speed over 30 minutes compared with controls, but only a 7% decline of out-loud reading speed.6
Independent mobility, which is critical to living outside of an assisted living or nursing home setting, is another function impacted by glaucoma progression. An increased risk for falls as a result of peripheral visual field loss is one of the primary factors leading to a more sedentary lifestyle.7 This can put patients at risk for heart disease, diabetes and bone thinning, among others.8
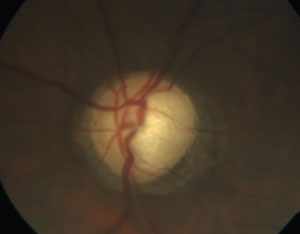 | |
| See the patient as more than just a glaucomatous nerve. Understanding and discussing glaucoma’s impact on their life will strengthen your rapport with the patient. Photo: Marta Fabrykowski, OD. |
Even if glaucoma patients remain active, they may be less so than their healthy counterparts: patients with glaucoma have been shown to participate in 3.2 minutes less (12.9 vs. 16.1 minutes) of moderate or vigorous physical activity and take 887 fewer steps (5,004 vs. 5,891 steps) than patients with normal vision.9 Patients with bilateral glaucoma also walk an average of 2.4m/minute slower around obstacles and experience 1.65 times the number of bumps, compared to those without glaucoma, according to research published in 2012.10 Interestingly, performance of those with unilateral glaucoma was not significantly different statistically compared with normal controls.10
Due to its effect on the patient’s peripheral vision, glaucoma can also impede safe operation of a motor vehicle. On average, every 5dB of visual field loss in the better eye doubles a patient’s odds of driving cessation.11 For those who drive despite vision loss, simulations show they are three times more likely to have an accident compared with normal controls.12
Treatment Adherence
Because they are faced with so many potential impacts to quality of life as a result of glaucoma progression, we’d expect patients to strictly adhere to their treatment regimen. Getting some patients to use their eye drops, however, is an uphill battle, especially if they do not believe vision loss will occur or if they have difficulty using—or even remembering to use—the drops.13
Lack of transportation to the pharmacy and the doctor’s office also impacts treatment adherence, as patients are severely deterred from refilling their prescriptions or attending follow-up visits. Conversely, those who travel more frequently are also less likely to take their drops due to the change in routine.
Five Tips For Improving Glaucoma Patients’ Medication Adherence
|
Patients with poor understanding of the disease and its progression are less likely to be compliant with administering their drops. Thus, it is imperative that doctors and patients communicate effectively. A study assessing interactions between doctors and patients found doctors typically did the majority of the talking during appointments (saying roughly 70% of the words) and asked two-thirds of the questions.14 The majority of these questions were closed-ended (94%), and patients were rarely questioned about their opinion or understanding of their disease and how it affected them.14 Thus, asking open-ended questions (i.e., “How are you doing with your drops?” rather than “Are you taking your drops?”) in a non-judgmental environment may help increase compliance.15 Improving educational efforts in the office may also improve understanding and subsequent compliance.16
Patients who need to administer glaucoma medicine more than twice daily and those who take different medications for multiple conditions are also less adherent to their glaucoma treatment regimen, research shows.17 Electronic monitoring of glaucoma patients also revealed that patients report higher medication use than their actual behavior; in fact, nearly 45% of patients who knew they were being monitored and who were receiving free medication used their drops less than 75% of the time.18 Research shows automatic reminders, either through a telecommunication-based system managed by the doctor’s office or patient self-initiation, improve compliance.15,19
With respect to compliance attending follow-up visits, noncompliant patients are: more likely to be suspects for glaucoma rather than exhibiting definite signs of the disease; be dissatisfied with the wait time for or cost of the examination; and be noncompliant with medicine use.20 Poor compliance with follow-up visits has been linked to increased disease severity.21
Dr. Fingeret is chief of the optometry section at the VA New York Harbor Healthcare System’s Brooklyn Campus. He is a founding member and past president of the Optometric Glaucoma Society.
1. Detry-Morel M. Currents on target intraocular pressure and intraocular pressure fluctuations in glaucoma management. Bull Soc Belge Ophthalmol. 2008:(308):35-43.2. Jampel HD. Glaucoma patients’ assessment of their visual function and quality of life. Trans Am Ophthalmol Soc. 2001;99:301-17.
3. Brown GC. Vision and quality-of-life. Trans Am Ophthalmol Soc. 1999;97:473-511.
4. Nelson P, Aspinall P, O’Brien C. Patients’ perception of visual impairment in glaucoma: a pilot study. Br J Ophthalmol 1999;83:546-52.
5. Ramuli PY, West SK, Munoz B, et al. Glaucoma and reading speed; the Salisbury eye evaluation project. Arch Ophthalmol. 2009 Jan:127(1):82-7.
6. Ramulu PY, Bonnielin KS, Jefferys JL, et al. Difficulty with out-loud and silent reading in glaucoma. Invest Ophthalmol Vis Sci. 2013 Jan;54(1):666-72.
7. Freeman EE, Munoz B, Rubin G, West SK, et al. Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci. 2007 Oct:48(10):4445-50.
8. Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006 Mar 14:174(6):801-9.
9. Friedman DS, Freeman E, Munoz B, et al. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology. 2007 Dec;114(12):2232-7.
10. Ramulu PY, Maul E, Hochberg C, et al. Real-world assessment of physical activity in glaucoma using an accelerometer. Ophthalmology. 2012 Jun:119(6):1159-66.
11. Ramulu PY, West SK, Munoz B, et al. Driving cessation and driving limitation in glaucoma: the Salisbury Eye Evaluation Project. Ophthalmology. 2009 Ot:116(10):1846-53.
12. Szlyk JP, Mahler CL, Seiple W, et al. Glaucoma and on-road driving performance. IOVS. 2008;49:3035-41.
13. Stryker JE, Beck AD, Primo SA, et al. An exploratory study of factors influencing glaucoma treatment adherence. J Glaucoma. 2010 Jan:19(1):66-72.
14. Friedman DS, Hahn SR, Quigley HA, et al. Doctor-patient communication in glaucoma care: analysis of videotaped encounters in community-based office practice. Ophthalmology. 2009 Dec;116(12):2277-85.
15. Chang JS, Lee DA, Petursson G, et al. The effect of a glaucoma medication reminder cap on patient compliance and intraocular pressure. J Ocul Pharmacol. 1991 Summer;7(2):117-24.
16. Friedman DS, Hahan SR, Gelb L, et al. Doctor-patient communication, health-related beliefs and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008 Aug:115(8):1320-7.
17. Gurwitz JH, Glynn RJ, Monane M, et al. Treatment for glaucoma: adherence by the elderly. Am J Public Health. 1993 May:83(5):711-6.
18. Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009 Feb;116(2):191-9.
19. Boland MV, Chang DS, Frazier T, et al. Automated telecommunication-based reminder and adherence with once-daily glaucoma medication dosing: the automated dosing reminder study. JAMA Ophthalmol. 2014 Jul:132(7):845-50.
20. Kosoko O, Quigley HA, Vitale S, et al. Risk factors for noncompliance with glaucoma follow-up visits in a residents’ eye clinic. Ophthalmology. 1998 Nov;105(11):2105-11.
21. Ung C, Murakami Y, Zhang E, et al. The association between compliance with recommended follow-up and glaucomatous disease severity in a county hospital population. Am J Ophthalmol. 2013 Aug;156(2):362-9.
22. Lichter PR, Musch DC, Gillespie BW, et al. CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943-53.
23. The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS), 7: the relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):42-40.
24. Heijl A, Leske MC, Bengtsson B, et al. Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-79.
25. Glaucoma Research Foundation. How compliance can help save your sight. www.glaucoma.org/treatment/how-compliance-can-help-save-your-sight.php.
26. Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011 Dec;118(12):2398-402.
27. Sleath B, Blalock SJ, Carpenter DM, et al. Ophthalmologist–patient communication, self-efficacy, and glaucoma medication adherence. Ophthalmology. 2014 Dec 24. [Epub ahead of print.].
28.American Academy of Ophthalmology. More than half of people with glaucoma skip or improperly administer medications, risking permanent vision loss. 2015 Jan. www.aao.org/newsroom/news-releases/detail/more-than-half-of-people-with-glaucoma-skip-improp#_edn3.

