Researchers at the Washington University School of Medicine in St. Louis have discovered a pathway that leads to the formation of atypical blood vessels, causing vision loss in patients with age-related macular degeneration.
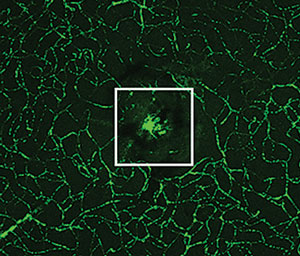 | |
| Normal blood vessels surround a clump of new, abnormal vessels that has formed beneath the center of the retina. Photo: Apte Laboratory, Washington University. |
The study, published online in the journal Nature Communications, looked at both engineered mice and eye tissue from patients treated in the 1980s and 1990s, when the removal of abnormal blood vessels was routinely performed on patients with wet AMD. The investigators found that, in both mice and human tissue, a signaling pathway involving the protein STAT3 was activating and altering immune cells, called M2 macrophages, known to contribute to the development of damaging blood vessels beneath the retina.
The researchers are hopeful the discovery could one day lead to targeted treatments, as some compounds can disrupt the actions of STAT3 in mice and keep the pathway from activating blood vessel growth. Those same compounds may also alter the course of macular degeneration in patients diagnosed with the condition, according to a Washington University press release.
“Now that we have a better idea of how these macrophages are activated at the molecular level, we may be able to use those drugs to halt or reverse the disease process,” says principal investigator and retina specialist Rajendra S. Apte, MD, PhD.
“This study mirrors a new trend in research that looks at inflammation and the immune system as mediators of age-related macular degeneration, specifically wet, or neovascular, AMD and choroidal neovascular membrane (CNVM) formation,” says Steven Ferrucci, OD, of the US Department of Veteran Affairs in North Hills, Calif., and a professor at the Southern California College of Optometry at Marshall B. Ketchum University in Los Angeles. “If the mediators of CNVM formation can be better understood, more targeted therapies may prove useful. Anti-VEGF therapy has been a great step in the right direction for AMD treatment, but monthly injection simply is not a sustainable treatment model. Newer therapies with different modes of action, synergistic medications, longer acting medication, alternative routes of administration, all need to be and are being investigated.”
Nakamura R, Sene A, Santeford A, et al. IL10-driven STAT3 signalling in senescent macrophages promotes pathological eye angiogenesis. Nature Communications. 2015;6:7847.
