|
|

|
Q: A 21-year-old white female, a regular contact lens patient, called my office with a complaint of recent-onset blurry vision. My office was booked up that day, and my front desk staff recommended the patient see her primary care doctor. We later learned that the primary care doctor told the patient she probably had a migraine.
Afterward, I happened to check this patient’s chart and saw that she had a history of lattice degeneration. Now I’m concerned. What can I do to make sure such a snafu doesn’t happen again?
A: “No matter what the patient’s complaint is—even if it’s itchy eyes—the staff should pull up the record at the time of the phone call,” says Steven Holbrook, OD, of The Eye Center of Southern Indiana.
Dr. Holbrook recounts the situation of a similar patient who wound up at his secondary-care center upon referral from the ER. In this young woman’s case, she too had called her eye doctor’s office with a complaint of sudden loss of vision and was referred to her PCP on suspicion of migraine.
|
|
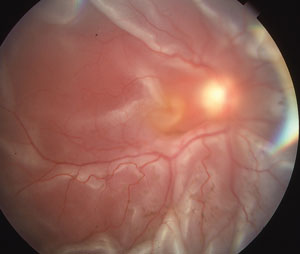
| The patient called complaining of sudden loss of vision. Turned out, she had a retinal detachment. |
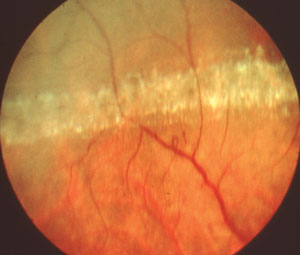
In the patient’s other eye, she had extensive lattice degeneration.
|
The patient’s symptoms worsened over the weekend and she went to the ER. A CT scan performed at the ER was negative and she was referred to Dr. Holbrook’s practice.
“When she came in to my office on Monday, I found she had a macula-off retinal detachment with hand motion vision. In her other eye, she had extensive lattice degeneration,” he says.
Dr. Holbrook sent the patient to a retina specialist, who performed a scleral buckle the next day. At the patient’s most recent follow-up visit, her visual acuity had im-proved to 20/150.
Had her original eye doctor seen the patient that day, the situation might have turned out much better.
As it is, “I feel so bad for this girl. In all likelihood, she’s going to have permanent vision loss,” Dr. Holbrook says. In these cases, every clinician should be able to look back at an old record and see the results of a dilated peripheral retinal exam.
Also, be sure to train your staff—with regular reminders—to check the record of every patient before making a recommendation, Dr. Holbrook says.

