|
|
 |
A 38-year-old Hispanic female from Honduras presented with a painless, sudden onset of blurred vision in the left eye of unknown duration. She stated that her central vision was most affected. She denied any pain, discomfort, flashes, floaters, nausea, fever or weight loss. She reported her right eye was unaffected.
Her past ocular history was unremarkable and she reported good health. She neither takes any medications nor has a history of any prior ocular trauma or surgeries. She was not nursing or pregnant.
Upon examination, her best-corrected visual acuity was 20/20 in her right eye and hand motion vision in her left eye. The confrontation fields were full to careful finger counting in her right eye and constricted in her left eye.
Ocular motilities were normal and her pupils were equal, round and responsive to light with no afferent pupillary defect. The anterior segment in the left eye was positive for trace cell, but otherwise normal in both eyes.
On dilated fundus exam, the right eye was unremarkable. The vitreous of the left eye was positive for 1+ vitreous cells with vitreal haze. Other changes are seen in figure 1. Lattice degeneration was present inferiorly in both eyes.
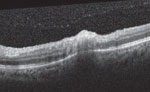
An SD-OCT of the macula in the left eye was obtained and is available for review (figure 2). An autofluorescence image (figure 3) was also obtained.
|
|

|
|
|
Fig. 1. Dilated fundus of the left eye.
|
Take the Retina Quiz
1. What do the fundus changes in the right eye macula show?
a. Papilledema.
b. “Headlights in the fog.”
c. “Snowballing.”
d. Macular star.
2. What additional testing would be most helpful in making the correct diagnosis?
a. Blood test for IgG and IgM.
b. Blood test for FTA-ABS, RPR.
c. PPD.
d. HLA-B27, HLA-A29.
3. What is the treatment for this patient?
a. Bactrim PO, clindamycin PO, steroids PO, folic acid.
b. Azithromycin PO.
c. Doxycycline PO.
d. Steroids IV.
4. What is most likely the diagnosis?
a. Histoplasmosis.
b. Tuberculosis.
c. Toxoplasmosis.
d. Toxocariasis.
For answers, see below.
Diagnosis
Our patient has a white, chorioretinal, inflammatory lesion with an overlying vitritis adjacent to a dark, chorioretinal scar. The lesion was directly overlying the macula. This presentation is more commonly known as “headlights in the fog,” which represents an active vitritis overlying a white foci of retinochoroiditis. Adjacent to the active lesions is an old chorioretinal scar from a previous active lesion. This presentation most likely represents ocular toxoplasmosis. The patient did not admit to having any cats nor eating any raw or undercooked pork, lamb or venison.
|
|
|
|
|
Fig. 2. OCT of the macula in the left eye.
|
Toxoplasmosis, the most common cause of posterior uveitis, accounts for approximately 90% of focal necrotizing retinitis.1 Toxoplasma gondii is a small, oblong shaped, intracellular protozoan parasite known to cause toxoplasmosis. The rate of seropositivity for toxoplasmosis is estimated around 22.5% in the United States.2 More than 60 million in the United States may have been affected by the parasite but, of those, few display symptoms.1 This is because a healthy immune system usually keeps the parasite from causing illness.
The diagnosis is usually made based on the clinical presentation. Blood work can be performed, but a positive result does not always ensure a diagnosis. Interestingly, there is a high seropositivity in the general population, which means that a positive titer does not necessarily confirm the diagnosis, but a negative titer should prompt strong deliberation of alternate diagnoses. IgG antibodies are produced within two weeks of infection and peak at two months, then later present for life.3 Detection of IgM antibody titers are usually possible within the first two weeks of infection and suggest a recently acquired infection.3 Blood work-up was not performed on our patient because it was a pretty “classic” presentation.
The disease can be transmitted via several potential methods. Ingesting undercooked meats such as pork, lamb or venison could be a culprit. Another involves consuming water contaminated with the parasite or accidental exposure through contact with cat feces. The most common transmission is mother-to-child (transplacentally).

|
|
|
Fig. 3. Autofluorescence of the left eye.
|
|
Mothers who are seropositive for toxoplasmosis show rates of transmission that range between 60% and 81%, which can be more noticeable in the third trimester.4 Manifestations of congenital toxoplasmosis include: hydrocephalus, seizures, intracranial calcifications and retinochoroiditis.
Clinical symptoms of active toxoplasmosis included blurred vision, floaters and potential redness or photophobia or both. Pain is typically absent, except with iridocyclitis. The clinical appearance of a toxoplasmosis lesion may vary depending on whether the infection is active or inactive. The active state usually appears as a unilateral, whitish, fluffy, retinal lesion with blurred margins. When the disease reoccurs, it often does so next to a “satellite lesion” also known as an old chorioretinal scar.
Toxoplasmosis is generally self-limiting in immunocompetent patients, and treatment is reserved for lesions threatening or involving the macular or optic nerve. We elected to treat our patient in two ways. Since the lesion was active and directly involving the macula and her vision was drastically affected, the patient was given an intravitreal injection of dexamethasone 0.4mg/clindamycin 1mg in office. Studies show that intravitreal injection of clindamycin and dexamethasone is as effective as conventional oral therapy in treatment of ocular toxoplasmosis with fewer systemic side effects.5 A study at the Nikookari Eye Hospital in Iran tested oral therapy vs. intravitreal for ocular toxoplasmosis, and within six months the results were equally effective in terms of increased BCVA, a decrease in lesion size and a termination of the vitritis.
After the injection, the patient was placed on clindamycin 30mg PO TID, Bactrim DS PO BID and prednisolone 40mg PO QD. She will continue this oral dosage for a month. At her two-week follow-up, the vitritis resolved and the acuity improved to 20/800 OS. The visual prognosis is guarded secondary to macular involvement. Spiramycin is reserved for fetal prophylaxis or to decrease disease severity in cases of maternal infection without fetal infection. It is prescribed as 1g every eight hours for the duration of pregnancy once diagnosed.4
In cases of confirmed infection of the mother and the fetus (through cranial ultrasound or amniocentesis), the mother is given oral Bactrim PO until delivery.
This case was written and provided by Nikolaos C. Zagorianos, OD, an optometric resident at Bascom Palmer Eye Institute.
1. Gerstenblith A, Rabin M. The Wills Eye Manual: office and emergency room diagnosis and treatment of eye disease, 6th edition. Philadelphia, Lippincott Williams & Wilkins 2012; 369-371.2. Yanhoff N, Duker J. Uveitis and Other Intraocular Inflammations” Ophthalmology: Expert consult, 3rd edition. Mosby November 2008; 828-831
3. Onofrey B, Skorin L, Holdeman N. Ocular Therapeutics Handbook: A clinical Manual, 3rd edition. Philadelphia, Wolters Kluwer Health, 2011; 477-481
4. Chaudhry S, Gad N, Koren G.Toxoplasmosis and Pregnancy. Can Fam Physician April 2014; PMCID: PMC4046541.
5. Baharivan N, Mahdavifard A, Fouladi R. Intravitreal clindamycin plus dexamethasone versus classic oral therapy in toxoplasmic retinochoroiditis: a prospective randomized clinical trial. Int Ophthalmology 28 September 2012. doi: 10.1007/s10792-012-9634-1
Retina Quiz Answers
1) b; 2) a; 3) a; 4) c.

