 |
A 64-year-old Hispanic female presented with complaints of blurred vision in both eyes for approximately six months. She explained that it was difficult to focus and her vision was hazy.
Her last eye exam was approximately three years ago, and she was given glasses at that time. She felt she was seeing well until about six months ago when she noticed her vision declining.
Her medical history is significant for pancreatic cancer, diagnosed seven months ago. She was on a course of chemotherapy with Abraxane (paclitaxel, Celgene) and Gemzar (gemcitabine, Eli Lilly).
On examination, her best-corrected visual acuity measured 20/80 in her right eye and 20/200 in the left. Her pupils were equally round and reactive to light; no afferent defect was seen. Confrontation visual fields were full to careful finger counting in both eyes, and ocular motility was normal. The anterior segment was significant for nuclear sclerosis in each eye. Intraocular pressure by applanation tonometry measured 17mm Hg in both eyes.
On dilated fundus exam, her optic nerves appeared healthy with small cups and good rim coloration and perfusion in both eyes. The vessels were normal caliber and her peripheral retinas were unremarkable. Of interest was the macula in each eye, which appeared thickened (see fundus photos). Fundus autofluorescence (FAF), spectral domain optical coherence tomography (SD-OCT) and fluorescein angiogram (FA) were obtained.
  | |
| Fundus photos (OD left, OS right) of our patient—what do you see in the macula? | |
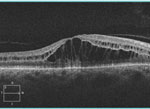 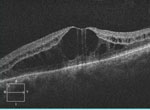 | |
| SD-OCT images (OD left, OS right)—what do these reveal? |
Take the Quiz
1. What does the SD-OCT show?
a. Cystoid macular edema (CME).
b. Vitreomacular traction (VMT) and CME.
c. Neurosensory retinal detachment.
d. Stage I macular hole development.
2. What do the fluorescein angiogram findings reveal?
a. Diffuse retinal thickening.
b. Essentially normal.
c. Cystoid macular edema.
d. VMT.
3. What is the correct diagnosis?
a. CME
b. Non-staining CME.
c. Diffuse macular edema.
d. VMT.
4. What is the likely etiology?
a. Metastasis from her pancreatic cancer.
b. Secondary to chemotherapy medications.
c. VMT.
d. Idiopathic.
5. How should this patient be managed?
a. Intravitreal anti-VEGF injection.
b. Topical steroid/NSAID.
c. Pars plana vitrectomy.
d. Change/discontinue chemotherapy medications.
For answers, see below.
Diagnosis
It was readily apparent on the clinical exam that our patient had macular thickening due to CME. In patients with CME, it is often difficult to see the cystic changes in the macula, but in our patient they were easily visible. We ordered an SD-OCT, FAF and FA to confirm the clinical diagnosis to provide baseline information for follow-up.
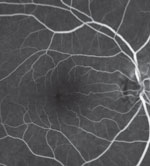 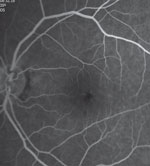 | |
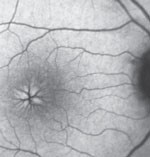
| Late fluorescein angiogram images (OD left, OS right). |
The SD-OCT shows clearly visible cystoid macular edema with the individual cystic spaces clearly delineated. These are highlighted on the FAF images, which show hyper-fluorescence of the cystic spaces surrounding areas of hypofluorescencene.
What is particularly interesting is the FA. On the FA, we expected to see late staining of the cystic spaces, which is what is seen with CME. However, in our patient, no such staining exists. This “non-staining” CME is most unusual and seen in rare conditions such as juvenile X-linked retinoschisis, Goldmann-Favre syndrome and niacin toxicity.
So what is going on with our patient?
The etiology of the non-staining CME is due to one of her chemotherapy agents, likely Abraxane. Abraxane is a member of the taxane family of microtubule stabilizing agents that has demonstrated clinical efficacy in multiple human malignancies.1 Toxic effects to bone marrow are the predominant dose-limiting adverse effect; however, ophthalmic adverse effects include decreased vision, scintillating scotomas and abnormal visual evoked potentials.
 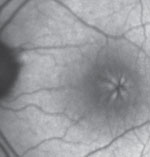 | |
| Fundus autofluorescence images (OD left, OS right). |
Non-staining CME from this drug was first reported in a 2007 publication, and others have since been reported.1,2
Advances in chemotherapeutic drug agents have improved survival for cancer patients. As a result, eye care providers may see more adverse ocular side effects from these antineoplastic medications. Because these side effect complications are so rare, it can be difficult to attribute ocular toxicity to a particular medication. It becomes even more difficult when patients are on combination chemotherapeutic agents, which is common in the management of cancer patients.
We explained our findings to the patient and notifed her physician. Her chemotherapy medications were stopped and she was put on a different regimen. We saw her a month later and her CME had resolved and her vision improved to 20/30 in each eye.
1. Joshi M, Garretson B. Paclitaxel maculopathy. Arch Ophthalmol. 2007;125:709–10.2. Koo N, Kim Y. A Case of Paclitaxel-induced Maculopathy treated with methazolamide. Korean J Ophthalmol. 2012 Oct;26(5):394–7.
Retina Quiz Answers:
1) a; 2) b; 3) b; 4) b; 5) d.

