 |
Q: A former patient contacted me recently complaining of visual disturbance. A retina specialist told her she needed a corneal evaluation for keratoconus, and sent her to yet another specialist. She called me to try and sort out the confusion. When I see a patient who just saw a specialist, am I off the hook from dilating?
A: “We know that you cannot assume the patient is giving you the entire story. In this case, the retinal specialist ‘said nothing about the fundus.’ However, you should never trust the history, or the assessment and plan of another eye doctor, until you verify it with your own eyes,” says Scott Moscow, OD, of Roswell Eye Clinic in Roswell, Ga. Doctors can miss things, or something new could have developed between visits. “You never know the full story without looking at the eye from front to back,” says Dr. Moscow.
To do this, Dr. Moscow advises dilating every patient who experiences unexplained vision loss. “The dilated fundus exam showed bilateral swollen discs! Who knows how long my patient would have gone on thinking she was losing vision from keratoconus?” Do not simply rely on the previous specialist—perform a dilated fundus exam on every new patient.
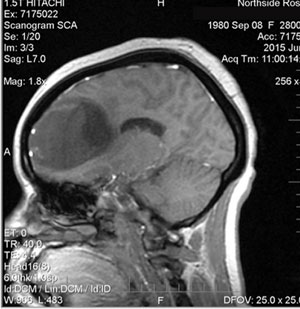 | |
| The patient’s constricted visual fields were due to a grade 3 astrocytoma of the left frontal lobe. |
Trust Your Gut
Other than mild headaches and slight lethargy, Dr. Moscow’s patient didn’t have neurological symptoms. Statistically, due to her age, weight and sex, he suspected idiopathic intracranial hypertension. “There were a few red flags that had me concerned,” Dr. Moscow says. The first: her visual acuities were 20/200-1 OD and 20/250 OS. Second, her visual fields were severely constricted. “Anecdotally, I don’t see visual acuities that poor, or visual fields constricted to that extent, when dealing with a case of idiopathic intracranial hypertension,” says Dr. Moscow.
Given these warning signs, Dr. Moscow scheduled the patient for an appointment with a neurologist the next day. “Although the next available appointment was more than three weeks away, I persisted and got her in after bypassing the receptionist, asking to speak directly to the doctor,” says Dr. Moscow. “I arranged an MRI that morning, prior to her appointment, in order to avoid further delays.” The patient did have intracranial hypertension, but it was not idiopathic: it was secondary to a space-occupying frontal lobe lesion.
Dr. Moscow emphasizes the critical importance of developing a relationship with any doctor to whom you refer your patients. “Direct communication was the key to getting a timely appointment and definitive diagnosis for this patient,” says Dr. Moscow. It is also important to make the appointment for the patient, and not leave it up to them. “She would have been told that the earliest appointment was almost a month away, and she might have had to accept that,” says Dr. Moscow. He says that it is also vital to listen to ‘your gut’—what your brain is telling you the data could mean. “My patient’s fundus appearance was stereotypical of ‘benign’ intracranial hypertension, if there is such a thing; however, the reduced visual acuities and fields were very atypical.”
In this case, Dr. Moscow says it was most important to look at the back of her eye rather than rely entirely on the patient and a previous specialist, who said that she was there “only to be fit with contact lenses for keratoconus.”
“Many, many problems can occur in the back of the eye that can only be viewed when dilated,” says Dr. Moscow. Just because they are under the care of someone else for another issue doesn’t mean that you abdicate responsibility or assume anything. “When a patient presents to your office, you are officially responsible for every problem they come in with.”
