
A 27-year-old female nursing student presents urgently for evaluation following an accident at work. She was reaching for a stack of papers high on a shelf when they fell down upon her; one sheet hit her in the face, giving her a paper cut across her right cornea. She went immediately to the emergency room, where she was diagnosed with a corneal abrasion and given a topical antibiotic solution to instill four times per day.
She did so dutifully, but she remained in agony through the rest of the day and into the night. She had so much pain that she couldnt sleep; she had to sequester herself to a darkened room with the shades drawn. The pain became so unbearable that she could not function. Now, she presents urgently for ophthalmic consultation.
Her best-corrected visual acuity is 20/200 O.D. She has a large central corneal abrasion, profuse corneal edema, folds in Descemets membrane and a modest anterior chamber reaction. There is no mucopurulent discharge or stromal infiltration to indicate corneal infection. The prescribed antibiotic was effective in preventing a secondary infection.
Why is the patient in such agony? Could it have been avoided? Clearly, the emergency room physician knew to provide prophylaxis against infection; however, the job doesnt stop there. What was overlooked: use of a cycloplegic agent.
When we were in training, our professors imparted a very important axiom that, to this day, we still teach to our students and residents: You cant go wrong to cycloplege. This simple saying has saved many patients from unnecessary suffering.
If a patient is in ocular pain for almost any reason (barring acute angle-closure glaucoma), and you arent sure how to manage the pain, the use of a cycloplegic agent would likely help and, at the very worst, slightly blur your patients vision. In this column, we examine the science behind cycloplegia to see if the old saying still holds true.
Mechanism of Action
Cycloplegics block the action of acetylcholine, a stimulatory neurotransmitter of the autonomic nervous system. So, they are known as anticholinergic or antimuscarinic drugs.1 In the eye, acetylcholine receptors are located within the iris sphincter muscle as well as the ciliary body. Activity of these receptors results in contraction of the iris and ciliary body. Cycloplegics temporarily inhibit this activity, causing ciliary body paralysis and pupillary mydriasis.
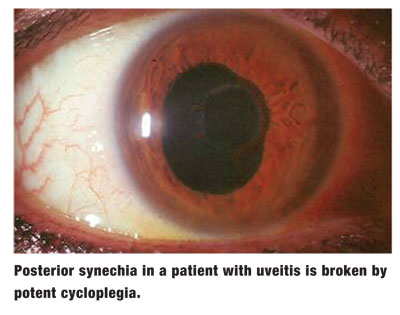
Cycloplegics are extremely effective in relieving pain caused by ocular inflammation; they relax ciliary spasm by paralyzing the muscle. Further, they help prevent posterior synechiae formation by decreasing the area of the posterior iris that contacts the anterior lens capsule when the pupil is dilated.2 Cycloplegics can also stabilize the blood-aqueous barrier, thus reducing the amount of cell and flare reaction in the anterior chamber. For these reasons, cycloplegics have long been used in the management of patients with corneal injury and uveitis, for example.3-6
Review of Cycloplegics
Atropine: This medication first was derived from the belladonna plant, Atropa belladonna, in 1831.1 Atropine is the most potent cycloplegic agent available clinically, with a duration of action lasting up to 12 days in a healthy eye. Atropine is available in 0.5%, 1%, and 2% ophthalmic solutions and a 1% ophthalmic ointment. A recommended regimen for atropine cycloplegia has been seven to 10 applications within three to four days; however, cycloplegia obtained after eight instillations was not greater than after four instillations in healthy eyes.7 Typically, dosing of atropine is b.i.d. in the affected eye. While atropine can usually be discontinued after a few days, more extensive usage may be required in highly inflamed eyes.
Scopolamine: Also known as hyoscine, this medication comes in 0.25% ophthalmic solution. Though scopolamine has a shorter duration of cycloplegia than atropine, its antimuscarinic activity is greater than that of atropine on a weight basis. Cycloplegia (as measured by accommodative ability) generally wears off within three days of treatment.8 Typical dosing is b.i.d. to t.i.d. in the affected eye.
Homatropine: This cycloplegic comes in 2% and 5% ophthalmic solutions and is typically dosed b.i.d. to t.i.d. Homatropine is only about one-tenth as potent as
atropine, and cycloplegic recovery occurs in one to three days.
While tropicamide and cyclopentolate are considered mydriatic or cycloplegic agents, we do not consider these to be therapeutic drugs and limit their use to diagnostic testing. Tropicamide is best used for routine pupillary dilation, and we have seen many practitioners fail to properly manage patients with uveitis because they used cyclopentolate as the cycloplegic agent. Cyclopentolate is not a strong enough cycloplegic agent when managing significant ocular inflammation, so it is best used for cycloplegic refractions on children. We like to say that, as far as cycloplegia is concerned, Cyclogyl is for kids.

Risks of Cycloplegia
The most feared complication of cycloplegic use is the potential for inducing acute angle-closure glaucoma from the mydriatic effect of these agents. A shallow anterior chamber is a risk factor that should be evaluated before inducing mydriasis and/or cycloplegia. The risk of precipitating an attack after evaluation should be minimal.9,10 One large population-based study saw the occurrence of acute angle-closure glaucoma following diagnostic mydriasis to be only 0.03%.11
Though uncommon, cycloplegics may induce mental and neurotoxic effects, and can even cause death in rare instances.12-15 The myriad of neurogenic symptoms induced by cycloplegic toxicity includes confusion, vivid visual hallucinations, restlessness, muscular incoordination, emotional lability, acute psychotic reactions, restlessness, excitement, euphoria, disorientation, stupor, coma and respiratory depression.12-15 But, these are rare, anecdotal reports. Exposure to cycloplegics should be taken into account in the differential diagnosis of acute confusional syndromes, and patients should be made aware of the rare possibility of these occurrences.
So, what became of our patient? The corneal abrasion appeared to be healing well, and the prescribed antibiotic was appropriate. So, we instilled two drops of scopolamine in-office and sent the patient home. Six hours later, we followed up with the patient by telephone, and she reported feeling remarkably well. She thanked us profusely for using the magic drop.
While in rare instances there can be untoward effects from cycloplegic use, this class of medication is extremely safe overall. Remember, when patients have ocular pain, you really cant go wrong to cycloplege.
1. Brown JH. Atropine, scopolamine and related antimuscarinic drugs. In: Gilman AG, Rall TW,
2. Wang T, Liu L, Li Z, et al. Ultrasound biomicroscopic study on changes of ocular anterior segment structure after topical application of cycloplegia. Chin Med J (Engl) 1999 Mar;112(3):217-20.
3. Janda AM. Ocular trauma. Triage and treatment. Postgrad Med 1991 Nov 15;90(7):51-2,55-60.
4. Torok PG, Mader TH. Corneal abrasions: diagnosis and management. Am Fam Physician 1996 Jun;53(8):2521-9,2532.
5. Wilson SA, Last A. Management of corneal abrasions. Am Fam Physician 2004 Jul 1;70(1):123-8.
7. Stolovitch C, Loewenstein A, Nemmet P, et al. Atropine cycloplegia: how many instillations does one need? J Pediatr Ophthalmol Strabismus 1992 May-Jun;29(3):175-6.
8. Marron J. Cycloplegia and mydriasis by use of atropine, scopolamine, and homatropine-paredrine. Arch Ophthalmol 1940;23:340-50.
9. Terry JE. Mydriatic angle-closure glaucomamechanism, evaluation and reversal. J Am Optom Assoc 1977 Feb; 48(2):159-68.
10. Brooks AM, West RH, Gillies WE. The risks of precipitating acute angle-closure glaucoma with the clinical use of mydriatic agents. Med J Aust 1986 Jul 7;145(1):34-6.
11. Wolfs RC,
12. Jimenez-Jimenez FJ, Alonso-Navarro H, Fernandez-Diaz A, et al. Neurotoxic effects induced by the topical administration of cycloplegics. A case report and review of the literature. Rev Neurol 2006 Nov 16-30;43(10):603-9.
13. Kortabarria RP, Duran JA, Chacon JR, et al. Toxic psychosis following cycloplegic eyedrops. DICP 1990 Jul-Aug;24(7-8):708-9.
14. Hamborg-Petersen B, Nielsen MM, Thordal C. Toxic effect of scopolamine eye drops in children. Acta Ophthalmol (Copenh) 1984 Jun;62(3):485-8.
15. Muller J, Wanke K. Toxic psychoses from atropine and scopolamine. Fortschr Neurol Psychiatr 1998 Jul;66(7):289-95.

