 |
 |
Patients want to improve their quality of life following cataract surgery and to be less dependent on corrective lenses after the procedure. During the cataract evaluation, patients must be informed of all available treatment options and ultimately decide which IOL option best suits their visual needs.
Every available IOL option comes with some sort of compromise, and patients must have realistic visual expectations. Many patients have spoken with friends or family members who’ve undergone surgery, and often hear “I don’t have to wear glasses.” What these patients don’t understand is that multiple variables involved in the preoperative work-up, including topography, biometry, IOL calculations, any presence of ocular pathology, and IOL selection, will directly contribute to individualized postoperative outcomes.
|
|
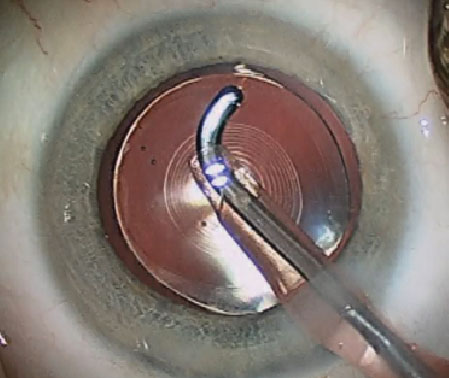
| Premium IOLs, such as this Alcon Restor multifocal, allow correction of near vision. Note the concentric rings of the diffractive optics visible centrally. |
A 2012 study found modern cataract surgery outcomes to be within +/- 0.50D of the target refraction in just 71% of cases.1 With many patients electing to pay out of pocket for premium IOLs, expectations are at an all-time high. And as consistent as we believe our cataract surgeons can be, isn’t it nice to know we can help to further perfect our patients’ surgical outcomes? Let’s review modern-day surgical techniques with phacoemulsification and clear corneal incisions.
Modern Cataract Removal
First, a paracentesis is created to provide access for the surgical instruments. Next, an injection of intracameral lidocaine and viscoelastic is placed into the anterior chamber to protect the corneal endothelium, manipulate tissues and maintain space during surgery.
Then, a secure, clear corneal incision is made to achieve a stable anterior chamber, minimize surgically induced astigmatism, provide adequate instrument maneuverability and prevent post-op wound leaks. This is followed by a continuous, curvilinear capsulotomy (capsulorhexis) to enable hydrodissection, prevent posterior capsule tears and allow for the implantation, fixation and centration of the IOL within the capsular bag. Hydrodissection is performed to reduce zonular stress during phaco by mobilizing the nucleus and epinucleus. Next, phacoemulsification fractures the cataract’s nucleus, which is followed by the removal of the remaining epinucleus and cortex with irrigation/aspiration.
Once complete, the IOL is implanted and centered within the capsular bag. Finally, the surgeon removes any remaining viscoelastic to minimize intraocular pressure spikes, then checks the clear corneal incision to ensure it is secure.
Be sure patients understand that many variables in the pre-op work-up (e.g., topography, biometry, IOL calculations, lens choice, any ocular pathology) influence outcomes. As a result, the approach will be highly individualized—and so will the results. Future columns will delve into how the technologies of modern cataract surgery address these patient-specific factors. Stay tuned!
1. Behndig A, Montan P, Stenevi U, et al. Aiming for emmetropia after cataract surgery: Swedish National Cataract Register study. J Cataract Refract Surg. 2012 Jul;38(7):1181-6.

