 Topical non-steroidal anti-inflammatory drugs, or NSAIDs as we typically call them, have been a valuable addition to the ophthalmic pharmaceutical arena for more than 25 years.
Topical non-steroidal anti-inflammatory drugs, or NSAIDs as we typically call them, have been a valuable addition to the ophthalmic pharmaceutical arena for more than 25 years.
In the body, NSAIDs work to diminish inflammation and mediate pain by inhibiting the cyclooxygenase (COX) enzymes. These enzymes catalyze the conversion of arachidonic acid into prostaglandins and thromboxanes––both powerful mediators of inflammation.
While not as potent a class of anti-inflammatory drugs as the corticosteroids, NSAIDs still possess a significant ability to ameliorate pain and reduce the signs of ocular inflammation, including postoperative cells and flare within the anterior chamber.1,2
 The Earliest Topical NSAIDs
The Earliest Topical NSAIDs
The first commercially available topical NSAID to receive FDA approval was Ocufen (flurbiprofen sodium 0.03%, Allergan) in 1986. Ocufen’s only indication was for inhibiting intraocular miosis during cataract extraction. But physicians who used this drug soon realized that it had an additional benefit––Ocufen also helped control some of the inflammation and pain following surgery.
When Voltaren (diclofenac sodium 0.1%, Novartis Ophthalmics) received approval in 1991, it was the first topical NSAID to carry a specific indication for postoperative pain. Then, Acular (ketorolac tromethamine 0.5%, Allergan) was granted FDA clearance in late 1992. While Acular was initially approved for the treatment of seasonal allergic conjunctivitis, it later secured approval for postoperative inflammation.
NSAIDs in Eye Care
Primary care optometrists use this class of medications far less frequently than our surgical counterparts in ophthalmology––particularly because the approved indication for these drugs is almost exclusively for the management of postoperative complications. Topical NSAIDs are currently accepted as the standard of care for postoperative management of cataract surgery, along with prophylactic antibiotics and corticosteroids.3
However, there are a number of off-label applications for topical NSAIDs, such as temporary relief of ocular pain due to superficial corneal insult. Because of their ability to inhibit prostaglandin synthesis, these drugs help to rapidly and effectively break the pain cycle.2
NSAIDs are used for corneal abrasions, corneal foreign bodies, recurrent corneal erosions and chemical keratitis, among others. Additionally, many optometrists are actively involved in the comanagement of surgical patients.
So, it’s important to understand the proper use of topical NSAIDs, including appropriate dosing and potential side effects. Knowledge of these drugs’ attributes also can help us make better decisions about drug selection and recommendation.
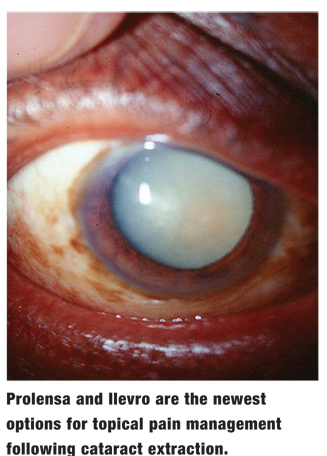 |
| Prolensa and Ilevro are the newest options
for topical pain management following cataract extraction. |
Over the years, improved formulation strategies have resulted in increased potency and diminished dosing requirements for this class of drugs, yielding more convenient and effective regimens. More recently, the FDA approved two new NSAIDs, Prolensa (bromfenac sodium 0.07%, Bausch + Lomb) and Ilevro (nepafenac 0.3%, Alcon).
• Prolensa. Bromfenac sodium has been a popular NSAID choice since 2005, when Xibrom (Bausch + Lomb) was first introduced in the United States. The halogenation of the bromfenac molecule with bromine is believed to impart increased potency and penetration into the ocular tissues. Prolensa actually contains a slightly lower concentration of bromfenac than its predecessors (Bromday and Xibrom both contained 0.09%). Like the previous formulations, it is preserved with 0.005% benzalkonium chloride (BAK).
Prolensa is indicated for the treatment of postoperative inflammation and reduction of ocular pain in patients who have undergone cataract surgery.4 The pH of Prolensa is 7.8, which is more physiologically neutral than that of Xibrom or Bromday (both 8.3).4-6 According to the manufacturer, this pH modification makes the bromfenac molecule more lipophilic and further improves penetration through the cornea.7
Although there currently are no head-to-head studies comparing Prolensa and Bromday, both once-daily formulations have been shown to be effective in managing postoperative inflammation in cataract patients.8
• Ilevro. Alcon’s Ilevro is a newer version of Nevanac (nepafenac sodium 0.1%, Alcon). Nepafenac is a prodrug of the more potent anti-inflammatory agent amfenac.9 In the body, prodrugs are converted to a more active drug state through enzymatic processes.10 Because nepafenac is a lipophilic, neutral molecule, some researchers have hypothesized that it may have greater corneal permeability than other NSAIDs that have acidic structures.9,11,12
Ilevro is indicated for the treatment of pain and inflammation associated with cataract surgery.13 In clinical trials, Ilevro dosed once daily was superior to its vehicle at completely clearing inflammation by day 14 post-op.14 In a similarly structured trial, Ilevro dosed once daily was found to be equivalent to Nevanac dosed TID.15 Both Ilevro and Nevanac are preserved with 0.005% BAK.
In addition to offering a 200% greater concentration of the active drug than its predecessor (0.3% vs. 0.1%), Ilevro has a number of other favorable attributes when compared to Nevanac. It has a lower pH (6.8 vs. 7.4), reduced molecule size, and demonstrates faster dissolution when instilled onto the ocular surface.16 Also, it contains several inactive ingredients that may help improve comfort, tolerability and ocular surface contact time––including guar gum, propylene glycol and carboxymethylcellulose.13
Although not one of the classes of drugs more commonly prescribed by optometrists, NSAIDs are a valuable addition to our pharmaceutical armamentarium and a crucial component of postoperative cataract management.
Additionally, NSAIDs help control intraoperative miosis, pain, inflammatory surgical complications, and perhaps even iatrogenic cystoid macular edema.17
In order to better serve our patients and communicate with our ophthalmologic colleagues, increased familiarity with the newest agents is essential.
Drs. Kabat and Sowka are consultants to Alcon. They have no direct financial interest in any of the products mentioned.
1. Henderson BA, Gayton JL, Chandler SP, et al. Safety and efficacy of bromfenac ophthalmic solution (Bromday) dosed once daily for postoperative ocular inflammation and pain. Ophthalmology. 2011 Nov;118(11):2120-7.
2. Donnenfeld ED, Nichamin LD, Hardten DR, et al. Twice-daily, preservative-free ketorolac 0.45% for treatment of inflammation and pain after cataract surgery. Am J Ophthalmol. 2011 Mar;151(3):420-6.
3. American Academy of Ophthalmology Cataract and Anterior Segment Panel. Preferred Practice Pattern Guidelines. Cataract in the Adult Eye. San Francisco: American Academy of Ophthalmology; 2011. Available at: www.aao.org/ppp. Accessed May 23, 2013.
4. Prolensa [package insert]. Tampa, Fla.: Bausch + Lomb Incorporated; 2013.
5. Bromday [package insert]. Irvine, Calif.: ISTA Pharmaceuticals, Inc.; 2010.
6. Xibrom [package insert]. Irvine, Calif.: ISTA Pharmaceuticals, Inc.; 2005.
7. Baklayan GA. 24-hour evaluation of the ocular pharmacokinetics of (14)C-labeled low-concentration, modified bromfenac ophthalmic solution following topical instillation into the eyes of New Zealand white rabbits. ARVO Meeting Abstracts; May 5, 2013. 54:123.
8. Gow JA, Goldberg DF, Peace JH, et al. Integrated phase III clinical trials of low-concentration, modified bromfenac ophthalmic solution dosed once daily for cataract surgery. Presented at the American Academy of Ophthalmology, Chicago. November 11, 2012. Poster: PO005.
9. Gamache DA, Graff G, Brady MT, et al. Nepafenac, a unique nonsteroidal prodrug with potential utility in the treatment of trauma-induced ocular inflammation. I. Assessment of anti-inflammatory efficacy. Inflammation. 2000 Aug;24(4):357-70.
10. Rautio J, Kumpulainen H, Heimbach T, et al. Prodrugs: design and clinical applications. Nat Rev Drug Discov. 2008 Mar;7(3):255-70.
11. Acosta MC, Luna C, Graff G, et al. Comparative effects of the nonsteroidal anti-inflammatory drug nepafenac on corneal sensory nerve fibers responding to chemical irriation. Invest Ophthalmol Vis Sci. 2007 Jan;48(1):182-8.
12. Walters T, Raizman M, Ernest P, et al. In vivo pharmacokinetics and in vitro pharmacodynamics of nepafenac, amfenac, ketorolac, and bromfenac. J Cataract Refract Surg. 2007 Sep;33(9):1539-45.
13. Ilevro [package insert]. Ft. Worth, Texas: Alcon Laboratories Incorporated; 2013.
14. Alcon Research. Confirmatory study nepafenac 0.3%. NLM Identifier: NCT01109173. Available at: http://clinicaltrials.gov/ct2/show/NCT01109173. Accessed May 23, 2013.
15. Alcon Research. Nepafenac 0.3% two study. NLM Identifier: NCT01318499. Available at: http://clinicaltrials.gov/ct2/show/NCT01318499. Accessed May 23, 2013.
16. Goldman DA. Ilevro––This Isn’t Your Father’s NSAID. Ophthalmology Web. Available at: www.ophthalmologyweb.com/Featured-Articles/136201-Ilevro-This-Isn-t-Your-Father-s-NSAID/. Accessed May 20, 2013.
17. Miyake K, Ota I, Miyake G, Numaga J. Nepafenac 0.1% versus fluorometholone 0.1% for preventing cystoid macular edema after cataract surgery. J Cataract Refract Surg. 2011 Sep;37(9):1581-8.

