The ruddy cheeks and prominent facial vessels that characterize rosacea are as obvious as they are distinctive. From W.C. Fields to Prince William to Bill Clinton, these patients are easy to identify. Less obvious, though, are the ocular signs—especially those that signal corneal involvement.
Rosacea is a relatively common disorder, affecting up to 10% of the adult population; it’s most frequently seen in those with fair skin and tends to manifest around facial folds.1-4 Middle-aged adults are most commonly affected, though children can also have this disorder.3,5 As many as 58% to 72% of rosacea patients have ocular involvement, and 45% to 85% have ocular complaints.1,3,4,6 The most frequently reported ocular signs are blepharitis and meibomian gland dysfunction, followed by conjunctival hyperemia—particularly interpalpebrally—eyelid margin telangiectasias, punctate epithelial keratopathy, corneal vascularization and infiltrates with corneal scarring and opacity.1,5 Ocular manifestations of rosacea may precede dermatologic signs in 20% of patients.1,3,6,7
 | |
| Ocular rosacea patient with typical eyelid findings, but also note the irregular corneal light reflex due to marked inferior corneal dryness. |
While our thoughts of ocular rosacea often end with the eyelids, corneal disease is often concomitant. It’s rare that ocular rosacea leads to marked or blinding corneal damage, but corneal involvement has been noted in up to 33% of patients with rosacea, and severe sequelae are possible.1,5 Be sure to look critically at the cornea and conjunctiva in these patients.
This article provides an overview of rosacea and how it affects the ocular surface.
An Uncertain Pathogenesis
Researchers have proposed many theories regarding the pathogenesis of rosacea, though none have been confirmed. The prevailing wisdom points to a mix of vascular and immunologic dysfunction.3,5 An increase in bacterial eyelid flora appears to have a strong contributory effect on ocular manifestations.
Bacteria produce several lipolytic exoenzymes—including cholesteryl esterase, triglyceride lipase and fatty wax esterase—that act on the lipid-based meibum by hydrolyzing its sterol esters and wax, thus increasing glycerides and free fatty acids.5,8 The latter are irritating and toxic to the ocular surface and adnexa.9,10 This process also alters the meibum’s solubility, causing it to thicken.9 Inadequate and solidified meibum destabilizes the lipid layer of the tear film, allowing the aqueous to evaporate more quickly, increasing tear osmolarity and stimulating the inflammatory cascade.4,5 Chronic inflammation causes atrophy of the meibomian glands themselves, decreasing meibum production.5,8,9 Symptoms associated with this process include burning or stinging, conjunctival and eyelid margin redness, foreign body sensation and often watery eyes from reflexive aqueous production.
Ocular rosacea patients also characteristically have an increased eyelid margin density of Demodex.11 An immune response to Demodex infestation on eyelash follicles and within meibomian glands also appears to contribute to chronic eyelid and meibomian gland inflammation and dysfunction.5,9 Demodex mites carry bacteria that produce proteins which stimulate an increased expression of matrix metalloproteinase (MMP) activity.9
Ocular rosacea is readily associated with blepharitis, eyelid margin telangiectasias, meibomian gland dysfunction and symptoms associated with dryness. Along with eyelid disease, researchers have also reported associations with conjunctivitis, chalazia, episcleritis, iritis, scleritis and scleral perforation.1
Corneal Complications
Up to 40% of patients with ocular rosacea may also display punctate epithelial erosions.5 This alone can cause a notable decline in vision and patient comfort. Peripheral stromal infiltrates are commonly seen with ocular rosacea; recurrent corneal erosions, ulcers, edema, stromal keratitis, opacification or scarring, neovascularization, pannus or phlyctenules may also occur.2,3,5,6 Limbal stem cell deficiency due to chronic inflammation may occur, resulting in inadequate corneal epithelial regeneration. Inflammation causes corneal epithelial cells to produce fibroblast growth factors and pro-angiogenic factors such as vascular endothelial growth factor (VEGF).12 In response, conjunctival endothelial cells produce more MMPs, and the limbal epithelial cells, which are capable of producing neovascularization and opacification, migrate beyond their normal limbal location onto the cornea.11,13 Additional immunologic cells are recruited, and this all contributes to triggering angiogenesis and corneal neovascularization.12
 | |
| Typical facial presentation with cutaneous rosacea; note rhinophyma, facial telangiectasias and eyelid findings. |
Ocular rosacea patients can have significantly increased tear concentrations of interleukin-1α (IL-1α), a pro-inflammatory cytokine, and matrix metalloproteinase 9 (MMP-9), a collagen matrix-degrading enzyme secreted by devitalized epithelial cells.5,14-17 Tear volume drops as IL-1α increases, and dry eye symptoms can worsen in the presence of elevated MMP-9 levels.14-16 InflammaDry (RPS), an in-office test that samples tears for elevated levels of MMP-9, could be a good confirmatory tool to help with early diagnosis and treatment. MMP-9 also overpowers inhibitory metalloproteinase proteins found naturally in the eye, leading to MMP-9’s degrading activity on the cornea, its epithelial basement membrane and stromal extracellular matrix, resulting in stromal thinning.14,15
In ocular rosacea, the inferior and intrapalpebral regions of the cornea are more susceptible to damage, particularly the 3- and 9- o’clock positions, due to the position of the tear meniscus inferiorly at rest and during a blink.5 Progressive corneal thinning and loss of stromal tissue can precipitate the formation of descemetocele; this herniation of Descemet’s membrane increases the risk of perforation.2,5 Rare corneal presentations such as dendritic keratopathy or features similar to keratoconus have been reported due to chronic ocular rosacea.2,14
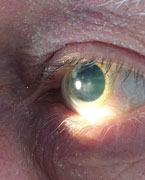  | |
| Another ocular rosacea patient with severe corneal involvement. Note the irregular corneal surface and corneal scarring. |
Managing Ocular Rosacea
Your role in helping patients live with this chronic disease is aimed at reducing pro-inflammatory contributors to the disease, controlling symptoms and reducing exacerbations. Management of ocular surface symptoms will include topical therapy, beginning with liberal lubrication with artificial tears. Inadequate lubrication can lead to abnormal corneal epithelial sloughing and corneal damage.
Furthermore, the avascular cornea needs many components of the tears for normal wound healing and reduced tear quality and quantity adds further insult.15 Lipid-based artificial tears make sense given the meibomian gland involvement.
More severe manifestations can be treated with autologous serum drops, which are rich in vitamin A, epidermal growth factor and fibronectin, which promote healthy development, proliferation, migration and differentiation of conjunctival and corneal epithelium; the serum contains bacteriostatic factors including lysozymes, complement and IgG.18,19 They are derived by centrifuging the patient’s whole blood (making them naturally non-allergenic) after it clots, reaping the plasma serum, filtering it and compounding it with preservative-free saline into the desired concentration; it’s packaged into single-use vials to be used liberally.18,19
Routine eyelid hygiene, massage and warm compresses are a mainstay. Devices for the expression of meibum are also available, which warm and massage the meibomian glands, improving meibum fluidity and flow onto the tear film.5 Thorough reviews of treatment for blepharitis, meibomian gland dysfunction and Demodex infestations are readily available elsewhere in the literature. Note that consistency with these lid considerations and liberal lubrication are foundational and cannot be overstated for preventing and managing both generalized rosacea and corneal manifestations of the disease.
| The Many Faces of Rosacea Rosacea is a chronic inflammatory dermatologic condition that affects the central face: most commonly the cheeks, forehead, chin and nose.1-3 Other than ocular rosacea, three subtypes and one variant exist2,3: Erythematotelangiectatic rosacea involves persistent flushing of the mid-face, which can occur with or without visible telangiectatic vessels. The central facial skin may be scaly or rough, mildly edematous and can often burn or sting.2 It is four times more common than the next most prevalent subtype, papulopustular.3 Sun exposure appears to significantly correlate with both its precipitation and severity.4 Papulopustular presents with papules or pustules or both overlying erythematous skin on the central face or around the nose, eyes or mouth. The papules and pustules may wax and wane, resembling acne vulgaris. It often occurs concomitantly with the erythematotelangiectatic presentation.2,3 Phymatous acne rosacea involves enlargement and thickening of the skin; this is most frequently seen as rhinophyma, but can also affect the cheeks, chin, forehead and even the ears. This subtype is generally uncommon, but is usually seen along with the other subtypes; it is more predominant in males.2,3 The variant granulomatous rosacea can be diagnosed even in the absence of other rosacea signs. It presents with non-inflammatory, hard cutaneous papules or nodules which can vary in color from yellow to brown to red; interestingly, they tend to appear over relatively normal, non-inflamed skin, but can lead to scarring.2,3 1. Kharod-Dholakia B, Loft ES, Song CD, et al. Ocular Rosacea. eMedicine. 18 Aug 2014. Available at http://emedicine.medscape.com/article/1197341-overview. 2. Wilin J, Dahl M, Detmar M, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584-7. 3. Tan J, Berg M. Rosacea: Current state of epidemiology. J Am Acad Dermatol. 2013;69(6):S27-S35. 4. Bae YI, Yun SJ, Lee JB, et al. Clinical evaluation of 168 Korean patients with rosacea: the sun exposure coorelates with the erythematotelangiectatic subtype. Ann Dermatol. 2009;21(3):243-9. |
Oral tetracyclines (doxycycline, tetracycline, minocycline) are the most effective treatment for dermatologic rosacea, and are also clinically useful in ocular rosacea.6 Interestingly, the antibiotic properties of the medication aren’t the main desired effect, but rather their anti-inflammatory actions. Tetracyclines, even at sub-antimicrobial levels, inhibit neutrophil chemotactic factors from bacterial flora, suppress pro-inflammatory cytokines and inhibit bacterial protein synthesis, therefore decreasing bacterial lipase and esterase.5-8,10,20 They also inhibit keratinization, and these effects are useful for the meibomian gland dysfunction associated with ocular rosacea.9 Tetracyclines also inhibit collagenase, an inflammatory product that degrades collagen, and suppress MMP-9 production.5,15 Thus, tetracyclines protect the cornea from the inflammation seen in ocular rosacea.6
Lastly, antiangiogenic effects, which can prevent corneal neovascularization, are achieved due to the inhibition of smooth-muscle cell migration and of vascular endothelial growth factor.7
In patients where tetracyclines are contraindicated (children, pregnant women, patients with hepatic dysfunction, or those who are allergic or intolerant), macrolides may be used; however, little clinical data supports their efficacy and tetracyclines are preferred.5
Oral antibiotics can be discontinued when symptomatic control is achieved or can be maintained chronically at low doses, with pulses as needed for exacerbations. Sub-antimicrobial dosages are typically for chronic use, and evidence of effective improvement in clinical signs and symptoms of the disease typically require around two months of treatment.5 Doxycycline is generally preferred over tetracycline due to its longer half-life, and therefore less frequent dosing.6 Doxycycline for ocular rosacea is typically dosed at 50mg to 100mg daily, though off-label and lower dosages—such as Oracea (Galderma Laboratories), a 40mg doxycycline tablet, 10mg of which is delayed-release, and Periostat (CollaGenex Pharmaceuticals), a 20mg formulation dosed twice daily—have been shown effective and are gaining popularity.3,6,7,21
Off-label use of topical ophthalmic antibiotics (such as erythromycin ointment) and antibiotic-steroid combinations are helpful in reducing eyelid bacterial proliferation, eyelid margin disease and meibomian gland dysfunction associated with ocular rosacea. Topical ophthalmic corticosteroids can be used in pulses for exacerbations. Chronic use is generally discouraged due to concern over steroid-induced corneal thinning or melting in an eye that is already at higher risk due to ocular rosacea-associated thinning and inflammation. Corticosteroids reduce the production of MMP-9 and other inflammatory products, so steroid use is a balance that needs to be monitored clinically; lower potency steroids are generally preferred when possible.6,15
 | |
| Typical eyelid findings with ocular rosacea; note eyelid margin keratinization and telangiectasias. |
Cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan) may be helpful as well. Similar to corticosteroids, cyclosporine reduces the production of inflammatory markers, including MMP-9.15,17 A clinical trial of topical cyclosporine in patients with ocular rosacea found that three months of use produced both symptomatic improvement and improvement in clinical signs, including tear production and degree of corneal staining.5,17 Other trials found a reduction in inflammatory markers after six months of cyclosporine use in patients with keratitis sicca and dry eye.15 This may be a very viable option for many ocular rosacea patients.
Other emerging treatments for severe corneal involvement include topical hormonal therapy such as dehydroepiandrosterone (DHEA) and medroxyprogesterone acetate (MPA). DHEA, an androgen, supports meibomian gland function.18 MPA, a synthetic progestin, inhibits MMP expression and interleukin-induced corneal collagen degradation by corneal fibroblasts.22 Their use is off-label, and there is limited evidence to date as to their efficacy.
Corneal neovascularization can be addressed in several different ways. Oral tetracyclines, as mentioned above, can play a preventative role, and topical corticosteroids or non-steroidal anti-inflammatory drugs can reduce the immunologic factors that trigger corneal neovascularization.12 Anti-VEGF agents bevacizumab and ranibizumab, which have made a profound difference in eye care, have been shown to reduce corneal neovascularization when applied via subconjunctival injection or with topical administration; however, long-term data is not available, route of delivery and dosing have not been standardized, and this is an off-label use of these drugs.12,23,24 Neovascularization could also be targeted with Nd:YAG or argon laser ablation, photodynamic therapy (PDT) or fine needle thermal cautery.12
| Don’t Forget Contact Lenses in Ocular Rosacea By Amy Lagina, OD Ocular rosacea has long been deemed a contraindication to contact lens wear. But we can often return these patients to safe contact lens wear by: (1) confirming the diagnosis, (2) working to treat the underlying disease, (3) addressing the eyelid and ocular surface factors and (4) carefully educating the patient on the do’s and don’ts. Mainstays of CL use in these patients are to protect the cornea and promote healing, or to alleviate symptoms. Specific goals can include vision correction, pain management, exposure and lid protection, and assistance with corneal reepithelialization. Contact lenses used for therapeutic purposes can be either bandage soft contact lenses or scleral gas permeable lenses. Continuous use of the approved lenses may vary from one to four weeks, depending on the ocular surface condition. Scleral lenses are common for the management of ocular surface diseases because they provide constant surface protection and enable more continuous lubrication. Scleral lenses are filled with a sterile saline prior to insertion and are fit to vault over the entire cornea, eliminating any interaction between the cornea and the lens.1 Lens materials with high oxygen transmissibility are recommended to prevent corneal hypoxia since scleral lenses are substantially thicker than standard gas permeable lenses. If the ocular surface presentation is mild and is properly managed, patients can continue to wear regular lenses. Important characteristics to consider when prescribing are: water content, oxygen permeability, ionicity, lens modulus, replacement schedule and maintenance. Ideal soft lenses have low water content, high oxygen permeability and a non-ionic surface. Soft HEMA (hydroxyethyl methacrylate) lenses will have decreased oxygen permeability as the lens dehydrates. Conversely, silicone hydrogel lenses will have increased oxygen permeability with lens dehydration. Silicone hydrogels also have high oxygen permeability, which significantly reduces the corneal hypoxia that can lead to contact lens discomfort.2 The ionicity is important to consider, as non-ionic lenses will have less protein accumulation and deposition. Lens modulus relates to the stiffness of the lens, with higher modulus lenses being stiffer, which generally creates more lens awareness. Most silicone hydrogel lenses have lower water content and a higher modulus, except Biofinity (comfilcon A 48%, CooperVision). Daily, two-week and monthly replacement lenses are becoming increasingly available. Daily lenses are ideal because they can be worn on an as-needed basis and discarded after each use. Finally, vigilant lens hygiene is important to prevent additional exacerbations with ocular rosacea. Reminding patients to rub their lenses nightly, use fresh solution daily, or switching to a hydrogen peroxide solution can greatly improve lens disinfection, compliance and overall success. Dr. Lagina practices at both the VA Ann Arbor Healthcare System and the Kellogg Eye Center in Ann Arbor, MI. She is a clinical instructor with the University of Michigan Department of Ophthalmology and Visual Sciences. 1. Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology. 2014;121:1398-1405. 2. Stapleton F, Papas E, et al. Silicone hydrogel contact lenses and the ocular surface. Ocul Surf. 2006;4(1):24-43. |
Severe corneal involvement in ocular rosacea may require surgical intervention. Corneal perforations require urgent ophthalmologic treatment, ranging from cyanoacrylate tissue glue to partial- or full-thickness keratoplasty.6 Severe neovascularization could also be a cause for corneal transplantation or the use of a keratoprosthesis.12 Because of chronic inflammation with ocular rosacea, post-keratoplasty patients may have an increased risk of graft neovascularization.5 The use of therapeutic amniotic membranes, which inherently have anti-inflammatory properties and promote healing and corneal epithelialization, may also be helpful in severe cases of ocular rosacea with corneal involvement.6
While the eyelids are more often involved in ocular rosacea, don’t forget the cornea! It’s involvement is potentially sight-threatening, so appropriate management is key.
Dr. Weidmayer practices at the VA Ann Arbor Healthcare System in Ann Arbor, MI. She is also a clinical instructor for the University of Michigan Department of Ophthalmology and Visual Sciences.
1. Ghanem VC, Mehra N, Wong S, Mannis M. The prevalence of ocular signs in acne rosacea. Cornea. 2003;22(3):230-3.2. Lee WB, Darlington JK, Mannis MJ, Schwab IR. Dendritic keratopathy in ocular rosacea. Cornea. 2005;24(5):632-3.
3. Donaldson KE, Karp CL, Dunbar MT. Evaluation and treatment of children with ocular rosacea. Cornea. 2007;26(1):42-6.
4. Onaran Z, Karabulut AA, Usta G, Örnek K. Central corneal thickness in patients with mild to moderate rosacea. Can J Ophthalmol. 2012;47(6):504-8.
5. Bron A. Ocular rosacea. Up To Date. 11 Dec 2013. Available at http://uptodate.com/contents/ocular-rosacea.
6. Kharod-Dholakia B, Loft ES, Song CD, et al. Ocular Rosacea. eMedicine. 18 Aug 2014. Available at http://emedicine.medscape.com/article/1197341-overview.
7. Sobolewska B, Doycheva D, Deuter C, et al. Treatment of ocular rosacea with once-daily low-dose doxycycline. Cornea. 2014;33(3):257-60.
8. Ta CN, Shine WE, McCulley JP, et al. Effects of minocycline on the ocular flora of patients with acne rosacea or seborrheic blepharitis. Cornea. 2003;22(6):545-8.
9. Mastrota K. Ocular surface disease. Optometric Management. 1 May 2009. Available at www.optometricmanagement.com/printarticle.aspx?articleID=102974.
10. Dougherty JM, McCulley JP. Bacterial Lipases and Chronic Blepharitis. Invest Ophthalmol Vis Sci. 1986;27(4):486-91.
11. O’Reilly N, Gallagher C, Katikireddy KR, et al. Demodex-associated bacillus proteins induce an aberrant wound healing response in a corneal epithelial cell line: possible implications for corneal ulcer formation in ocular rosacea. Invest Ophthalmol Vis Sci. 2012;53(6):3250-9.
12. Chiang HH, Hemmati HD. Treatment of Corneal Neovascularization. Eye Net Clinical Pearls. 2013;35-6.
13. Kim BY, Rias KM, Bakhtiari P, et al. Medically reversible limbal stem cell disease. Ophthalmol. 2014;121(10):2053-8.
14. Dursun D, Piniella AM, Pflugfelder SC. Pseudokeratoconus caused by rosacea. Cornea. 2001;29(6):668-9.
15. Kaufman HE. The practical detection of MMP-9 diagnoses ocular surface disease and may help prevent its complications. Cornea. 2013;32(2):211-6.
16. Kaufman HE. MMP-9 and its role in dry eyes. Advanced Ocular Care. 2011;40-2.
17. Schechter BA, Katz RS, Lriedman LS. Efficacy of topical cyclosporine for the treatment of ocular rosacea. Adv Ther. 2009;26(6):651-9.
18. Reed K. Dry eye treatment: the unusual suspects. Review of Cornea and Contact Lenses. March 2013. Available at www.reviewofcontactlenses.com/content/d/dry_eye/c/39490/.
19. Mangan R, Lehman S. How (and why) to make autologous serum. Review of Optometry. March 2012. Available at www.reviewofoptometry.com/content/d/dry_eye/c/33139/.
20. Stone DU, Chodosh J. Oral tetracyclines for ocular rosacea: an evidence-based review of the literature. Cornea. 2004;23(1):106-9.
21. Shovlin JP. Which antibiotic for rosacea? Review of Optometry. March 2007. Available at www.reviewofoptometry.com/content/d/cornea/c/15521/.
22. Zhou H, Kimura K, Orita T, et al. Inhibition by medroxyprogesterone acetate of interleukin-1β-induced collagen degradation by corneal fibroblasts. Invest Ophthalmol & Vis Sci. 2012;53(7):4213-9.
23. Chang J-H, Garg NK, Lunde E, et al. Corneal neovascularization: an anti-VEGF therapy review. Surv Ophthalmol. 2012;57(5): 415-29.
24. Stephenson M. Anti-VEGF for CNV: questions remain. Review of Ophthalmology. Sept. 2011. Available at www.reviewofophthalmology.com/content/i/1628/c/29956/.

