In our estimation, only about 30% to 40% of optometrists actively comanage cataract surgery postoperatively. Numerous factors contribute to this number, such as insurance, practice modality, patient demographics and possibly a lack of surgeons willing to “share care” (keep looking, because many will). But optometry needs to play a bigger role in pre- and postoperative care to meet patient demands and ensure best outcomes. 

Risks of Surgery
As safe as cataract surgery is, it still carries risk. The preoperative evaluation and patient education are keys to ensuring patients have realistic expectations. By addressing issues preoperatively we can minimize postoperative concerns. Here are four of the most common conditions that affect our patients’ vision postoperatively:
Cystoid Macular Edema (CME) is the most common cause of visual decline following uncomplicated cataract surgery. The development of CME is due in part to prostaglandin-mediated breach of blood-retinal barrier. It is estimated to occur in 1% to 3% of low-risk cataract cases with an onset of four to six weeks postoperatively.1 CME should be considered in patients who present with best corrected visual acuity (BCVA) worse than the previous examination. For patients at higher risk for CME, topical NSAIDs are prescribed one week prior to surgery. Treatment includes topical NSAIDs, oral steroids, periocular steroid injections, and pars plana vitrectomy.
The development of Posterior Capsular Opacification (PCO) is due to a proliferation of equatorial lens epithelium along the posterior capsule, which appears as a cloudy membrane. Symptoms include decreased BCVA, foggy vision and glare. The incidence of PCO is 10% to 25% and may present weeks, months or even years after the procedure.2 It is easily treated with a YAG laser capsulotomy.
 | |
| Keep any eye out for dry eye, which is commonly seen perioperatively. |
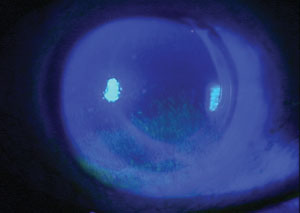
Ocular Surface Disease (OSD) is the most common reason for decreased vision after surgery. We cannot overemphasize the importance of aggressively treating OSD preoperatively. Studies show the incidence of dry eye is 80% of patients preoperatively and 87% of patients postoperatively.3-5 Consider OSD in patients who complain of fluctuating vision, burning or irritation after surgery. Signs include decreased tear film break-up time, corneal staining, increase OSD index scores, MGD and increased osmolarity and MMP-9 levels. Contributing factors include topical anesthesia, multiple eye drops with preservatives, light exposure and corneal incisions. Treatment includes artificial tears, nutraceuticals, topical anti-inflammatories and punctal occlusion.
Patient expectations are at an all-time high for cataract surgery, especially elective procedures such as femtosecond laser surgery coupled with premium IOL technology. Education on realistic outcomes is important—and that includes the possibility of residual refractive error. Patients may need a spectacle prescription for full-time wear or for certain activities. Discuss with your surgeon how to manage patients with residual refractive error after toric or multifocal implants. Many offer enhancements with laser refractive surgery or limbal relaxing incisions, which is included in the elective surgical fee.
Wrapping it All Up
With more than three million cataract procedures performed annually, optometrists play a key role in preparing patients for surgery and managing their care perioperatively. All complications, no matter the issue, should be discussed with your surgical team. Communication is key both pre- and postoperatively, and having everyone on the same page will help ensure the best possible outcomes.
2. Schaumberg D,. et al. A systematic overview of the incidence of posterior capsule opacification. Ophthalmology. 1998;105(7):1213-21.
3. Trattler WB, Reilly CD, Goldberg DF, et al. Clinical study report: Cataract and dry eye: prospective health assessment of cataract patients ocular surface study. Poster, ASCRS/ASOA Symposium & Congress. San Diego; March 2011.
4. Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight. 2007;32(1):14-23.
5. X-M Li, et al. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9)S1:S16-20.

