 |
Giant cell arteritis (GCA), also known as temporal arteritis, is the most common vasculitis in adults older than 50 years, with an incidence of approximately 18 per 100,000 per year.1 It affects women four times more often than it affects men and has a prevalence that is highest in caucasians, especially those of Scandinavian or Northern European decent.2-4
The disease is a vasculitis affecting medium and large-sized vessels that commonly, although not exclusively, develop in the superficial temporal artery and other extra-cranial branches of the carotid artery. This explains why a headache is the most common symptom associated with GCA.5
Often, GCA can develop into sudden vision loss and is considered a true ocular emergency. This article reviews the sequelae, diagnosis and treatment of GCA.
AAION
A highly-feared sequelae of GCA involves sudden, painless and profound vision loss in one or both eyes secondary to arteritic anterior ischemic optic neuropathy (AAION).6,7 A study estimates that one out of five patients diagnosed with GCA
 | |
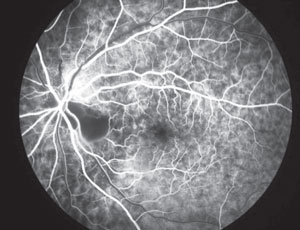
| Fig. 1. Optic nerve and retinal ischemia consistent with AAION and GCA. |
will develop monocular vision loss related to AAION, with more than one-third experiencing one or more episodes of transient vision loss prior to the event.6 Vision is often count fingers or worse and is accompanied by a pronounced afferent pupillary defect. If left untreated, approximately 50% will go on to lose vision in the fellow eye within days to weeks of onset.8 AAION secondary to GCA is considered a true ocular emergency.
In the acute phase, the optic nerve will appear swollen and pale (figure 1), often associated with flame-shaped hemorrhages.
Later, as the swelling subsides, optic atrophy sets in. Other signs that may be associated with AAION include cotton wool spots, central retinal artery occlusion, branch retinal artery occlusion and cranial nerve involvement (especially CN VI). The affected eye will often show an altitudinal visual field defect, but arcuate and cecocentral scotoma’s have also been reported.
Case History
Perform a thorough and careful case history when confronted with an acute ischemic optic neuropathy. While GCA most commonly affects patients older than 65 years, be on the lookout for this condition in any patients older than 50 years who complain of antecedent or simultaneous temporal head pain, scalp tenderness and jaw claudication (pain with chewing). Proximal muscle and joint pain (polymyalgia rheumatica), as well as constitutional symptoms such as fatigue, sweating, fever and weight loss, should raise suspicion for GCA. It is important to note, however, that approximately one out of every five patients who present with visual loss secondary to AAION do so without any systemic complaints.
Diagnosis
How important is it to confirm the diagnosis through temporal artery biopsy before starting treatment?
 | |
| Fig. 2. Fluorescein angiography typically shows delayed choroidal and central retinal artery filling, with possible choroidal nonperfusion, especially in the peripapillary area. |
Initiation of oral or IV steroids can adversely affect the results of a temporal artery biopsy, the gold-standard diagnostic procedure in confirming GCA.10 However, when dealing with visual symptoms or sudden severe vision loss in one eye related to AAION, waiting for a biopsy result is not an option. Given the potentially devastating consequences of delaying treatment, order bloodwork (CBC, ESR, CRP, FBS, FTA-ABS and ANA) and initiate treatment immediately, ideally in cooperation with a specialist in internal medicine or rheumatology.
Studies show that if aggressive steroid treatment is initiated within the first 24 hours of the onset of visual symptoms, the patient has a better than 50% chance of obtaining some improvement in vision. A delay in treatment drops these odds to approximately 5%.11
A temporal artery biopsy should still be ordered and ideally performed within one week of starting steroids. Evidence suggests that immediate treatment does not usually confound biopsy results within this time frame and in some cases for as long as three weeks out.12
False Negatives
Note that not all patients with GCA will have abnormal labs. Fifteen percent to 30% of patients with positive temporal artery biopsies have a normal ESR.13-15 It is also important to note that biopsy of the temporal artery carries a significant false negative rate (5% to 9%) due to skip lesions.16
Table 1. Physical Examination
|
The American College of Rheumatology (ACR) has developed a five-point scoring system with equal weighting for each of the following five parameters for GCA diagnosis:17
- Age more than 50 years.
- A Westergren ESR greater than 50.
- Temporal artery tenderness or abnormality on exam (table 1).
- New-onset headache.
- Positive temporal artery biopsy.
If three out of five are considered positive, this carries a sensitivity (93.5%) and specificity (91.2%) that distinguishes GCA from other forms of vasculitis.18 Therefore, even in cases where the ESR and biopsy results are inconclusive, patients that present with an AAION and have the other risk factors listed here should be treated promptly.
IV vs. Oral Steroid Delivery
Research has yet to clearly establish the benefits of IV methylprednisolone vs. oral steroids with respect to improved visual recovery. Some studies report improved visual recovery with IV delivery while others report no difference.19-20
The case for IV administration of methylprednisolone instead of oral administration of steroids is based more on the importance of prompt initiation of treatment and control of side-effects from treatment rather than better outcomes. First, compliance is 100% when medication is given intravenously. Also, drugs are typically more potent and act faster when delivered intravenously. Studies suggest that patients started on a three-day induction dose of IV methylprednisolone, 15mg/kg/d (about 1g per day), followed by oral prednisolone therapy (40 to 60mg/d) are able to be weaned off oral steroids faster than when placed on oral treatment alone.20 Patient tolerance of IV methylprednisolone is similar to that found with oral administration.
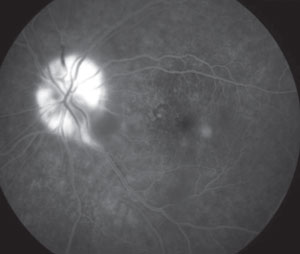 | |
| Fig. 3. In the late phase of the angiogram, leakage of dye is bound by the area of optic disc swelling. |
What is generally agreed upon is that patients with transient or persistent vision loss need immediate treatment by either delivery method, whichever will be most timely. In general, therapy with high-dose oral steroids is necessary for several weeks and is then followed by a slow taper and maintenance dosing to maintain a low ESR and CRP.21
Prognosis
The main goal of treatment is to prevent involvement of the fellow eye and other systemic vascular complications such as stroke or myocardial infarction. While some anecdotal cases report significant visual improvement with prompt treatment, the prognosis for visual recovery from AAION is generally poor. In fact, 30% of patients will continue to suffer visual decline despite aggressive IV methylprednisolone treatment.22
Risk factors for progressive visual loss despite steroid therapy include an elevated CRP, older age, and significant optic disc swelling.23
Giant cell arteritis is a severe inflammatory condition that can lead to stroke, blindness, and heart attack. Two thirds of patients with GCA offer a chief complaint of headache or temporal head pain. Knowing the other signs, symptoms, and risk factors for GCA may allow you to act in time so as to avoid serious complications, like blindness, from happening on your watch.
1. Unwin B, Williams C, Gilliland W. Polymyalgia rheumatica and giant cell arteritis. Am Fam Physician 2006;74:1547–54.2. Eberhardt R, Dhadly M. Giant cell arteritis: diagnosis, management, and cardiovascular implications. Cardiol Rev 2007;15:55–61.
3. Smith C, Fidler W, Pinals R. The epidemiology of giant cell arteritis: report of a ten-year study in Shelby County, Tennessee. Arthritis Rheum 1983;26:1214–19.
4. Wernick C, Duvey, M, Bonafede, P. Familial gianct cell arteritis: report of an HLA-typed sibling pair and review of the literature. Clin Exp Rheumatol 1994;12:63-6.
5. Salvarani C, Cantini F, Bolardi L, Hunder G. Polymyalgia rheumatica and giant-cell arteritis. N Engl J Med 2002;347:261–71.
6. Gonzales-Gay M, Blanco R, Rodriguez-Valverde V, et al. Permanent visual loss and cerebrovascular accidents in giant cell arteritis: predictors and response to treatment. Arthritis Rheum 1998;41:1497–504.
7. Liozon E, Ly K, Robert P. Ocular complications of giant cell arteritis. Rev Med Interne. Jul 2013;34(7):421-30.
8. Weyand C, Goronzy J. Giant-cell arteritis and polymyalgia rheumatica. Ann Intern Med 2003;139:505–15.
9. Hayreh SS, Podhajsky PA, Zimmerman B. Occult giant cell arteritis: ocular manifestations. Am J Ophthalmol 1998;125:521–26.
10. Ray-Chaudhuri N, Kine D, Tijani SO, et al. Effect of prior steroid treatment on temporal artery biopsy findings in giant cell arteritis. Br J Ophthalmol 2002;86:530–2.
11. Fraser J, Weyand C, Newman N, Biousse V. The Treatment of Giant Cell Arteritis. Rev Neurol Dis. 2008;5(3):140–52.
12. Achkar AA, Lie JT, Hunder GG, et al. How does previous corticosteroid treatment affect the biopsy findings in giant cell (temporal) arteritis? Ann Intern Med 1994;120:987–92.
13. Huston K, Hunder G, Lie J, et al. Temporal artertitis: a 25-year epidemiologic, clinical, and patholgic study. Ann Intern Med 1978;88:162-67.
14. Smetana G, Shmerling, R. Does this patient have temporal arteritis? JAMA 2002;287:92-101.
15. Hayreh S, Podhajsky, P, Raman, R, Zimmerman, B. Giant cell arteritis: validity and reliability of various diagnositic criteria. Am J Ophthalmol 1997;123:285-96.
16. Gonzalez EB. Arteritis associated with systemic disease. Coron Artery Dis 1995;6:207–12.
17. Hunder G, Bloch D, Michel B, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 1990;33:1122–8.
18. Haist S. Stroke after temporal artery biopsy. Mayo Clin Proc 1985;60:538.
19. Chevalet P, Barrier J, Pottier P, et al. A randomized, multicenter, controlled trial using intravenous pulses of methylprednisolone in the initial treatment of simple forms of giant cell arteritis: a one-year follow-up study of 164 patients. J Rheumatol 2000;27:1484–91.
20. Mazlumzadeh M, Hunder G, Easley K, et al. Treatment of giant cell arteritis using induction therapy with high-dose corticosteroids: a double-blind, placebo-controlled, randomized prospective clinical trial. Arthritis Rheum 2006;54:3310–18.
21. Hayreh S, Zimmerman B. Management of giant cell arteritis. Our 27-year clinical study: New light on old controversies. Ophthalmologica 2003; 217: 239–59.
22. Danesh-Meyer H, Savino P, Gamble G. Poor prognosis of visual outcome after visual loss from giant cell arteritis. Ophthalmology 2005;112:1098–103.
23. Loddenkemper T, Sharma P, Katzan I, Plant GT. Risk factors for early visual deterioration in temporal arteritis. J Neurol Neurosurg Psychiatry. Nov 2007;78(11):1255-9.

