A
weekly e-journal by Art Epstein, OD, FAAO
Off the Cuff: Antisocial Distancing and Other Viral Thoughts
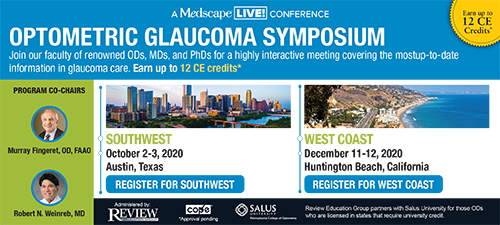
What a long strange trip this has been and, unfortunately, continues to be. While things continue to change almost daily, our experts remain confused, and the more we learn, the less we seem to actually know. For optometry, the COVID-19 outbreak has been a pressure test, and the insights we’ve gained can be valuable—if we view them with an open mind. With offices shuttered or severely limited, many colleagues faced unprecedented economic hardship. For those who clung to traditional refractive optometry as their primary source of income, the harsh reality of zero income meeting fixed expenses was a lot to bear. In some cases, it may have been too much. Economic challenges appeared to prompt some of the larger chain operations like Visionworks to expand the meaning of “essential care” to conflate it with urgent and emergency care. One lesson learned is just how vulnerable many practices are and how important it is to have cash reserves. I suspect it also marks the end of the equity capital gold rush with practice values in the dumps for the foreseeable future. One interesting aspect of the outbreak was how quickly live in-person CE ended and virtual CE began. With Vision Expo East postponed and Optometry’s Meeting canceled, the rapid transition was necessary, but it also was a real-time proof of concept of just how effective online CE can be. Don’t get me wrong. I love speaking at live meetings. It has defined much of my career, but it’s time that we look at how technology has made virtual programs effective and convenient. I realize that the thought of losing the CE income stream is terrifying to many groups. But the truth is that optometry has too many meetings, and we can and must find other ways to support our professional organizations. The COVID outbreak highlighted just how important it is for state boards to relax their strangleholds on virtual CE. It’s also well past time ARBO and COPE revised educational standards to allow parity between online and live CE. Also under pressure during the outbreak were our national and state organizations. Some did extremely well, while, from reports of colleagues, others not so much. The AOA did an outstanding job doing what it does best, supporting the profession operationally and legislatively. The American Academy of Optometry was a bit slow out of the gate, especially when countering misinformation about contact lens safety, but was great supporting student education. One thing that was sadly apparent was that our national organizations combined did not have anywhere near the clout of the American Academy of Ophthalmology, which used the coronavirus outbreak to lob hand grenades at optometry. During the first weeks of the outbreak, the MD academy was able to gain front-page headlines falsely attacking contact lens safety on both CNN and Fox News, as unlikely a media pair as could be. More recently, “How to Test Your Vision (and Order Lenses) at Home, According to Doctors” was a hatchet job appearing in New York magazine. I’ve written about this before, but the COVID outbreak has made it painfully apparent. The American Academy of Optometry’s lack of political wherewithal and the AOA’s absence of recognized world-class clinical expertise has hobbled the profession. It’s time we seriously considered getting past the egos and combining the two organizations. If they can’t find the path to an amalgam on their own, leaders in the profession need to form an independent committee to facilitate this. The profession’s future depends on it.Finally, I haven’t forgotten about Optometric Physician Live. More to come…
|
|||||
 |
||
| Short-term, High-dose Hydroxychloroquine Corneal Toxicity | ||||
This case report described the corneal findings and management of a 61-year-old female with vortex keratopathy following short-term, high-dose hydroxychloroquine used in the setting of a clinical trial for recurrent breast cancer. The patient was found to have significant corneal vortex keratopathy without retinal pathology within three months of 1,200mg daily hydroxychloroquine treatment as an adjuvant medication for cancer therapy. Cessation of the medication led to the resolution of the corneal verticillata within one month, yet the vision did not return to baseline. Ultimately, remaining irregular astigmatism and ocular surface disease required a scleral contact lens to achieve a BSCVA of 20/25 OU. |
||||
SOURCE: Savage DE, Plotnik R, Wozniak RAF. Short-term, high-dose hydroxychloroquine corneal toxicity. Am J Ophthalmol Case Rep. 2020;18:100713. |
||||
 |
||
| Clear Lens Extraction in Eyes with Primary Angle Closure and Primary Angle-closure Glaucoma | ||||
The crystalline lens plays an important role in the pathophysiology of primary angle closure (PAC) and primary angle-closure glaucoma (PACG). The aging process is associated with a progressive enlargement of the lens, resulting in greater iridolenticular and iridotrabecular contact, which exacerbates both pupillary block and appositional angle closure, irrespective of the cataract status of the lens. Cataract surgery has been shown to widen the angle and reduce intraocular pressure in eyes with PAC or PACG. Recently, clear lens phacoemulsification has been suggested as a treatment modality in such eyes. The authors reviewed the literature on clear lens extraction in eyes with angle closure, and discussed its efficacy, safety and indications. Although, they wrote, it is evident that clear lens extraction is beneficial in eyes with PAC and PACG, it is technically challenging and should be performed by experienced surgeons who not only master the procedure, but are also able to deal with potential complications. Authors wrote, since the follow-up of the reviewed studies was relatively short, long-term follow-up (>10 years) of patients who undergo this procedure would be needed to evaluate the safety and confirm the early benefits reported. |
||||
SOURCE: Costa VP, Leung C, Kook MS, et al; Global Glaucoma Academy. Clear lens extraction in eyes with primary angle closure and primary angle-closure glaucoma. Surv Ophthalmol. 2020; Apr 24. [Epub ahead of print]. |
||||
| Genotype and Phenotype-based Subgroups in Geographic Atrophy Secondary to Age-related Macular Degeneration: the Eye-risk Consortium | ||||
Geographic atrophy secondary to age-related macular degeneration (GA) is considered a single entity. This study aimed to determine whether there are GA subgroups that can be defined by their genotype and phenotype. |
||||
SOURCE: Biarnés M, Colijn JM, Sousa J, et al.; EYE-RISK Consortium. Genotype and phenotype-based subgroups in geographic atrophy secondary to age-related macular degeneration. The EYE-RISK Consortium. Ophthalmol Retina. 2020; May 1. [Epub ahead of print]. |
||||
| News & Notes | ||||||||
| Icare USA Launches Two New Devices Icare USA released two new diagnostic technologies: the Centervue DRSplus confocal fundus imaging system and the Icare ic200 handheld tonometer for portable measurement of intraocular pressure. The DRSplus confocal fundus imaging system uses white LED illumination, including the entire visible spectrum, to produce TrueColor and detail-rich images. Physicians can view detailed 45-degree retinal images as well as panoramic 80-degree images using the Mosaic function. The Icare ic200, based on a rebound measuring principle, measures IOP without anesthetic drops, air puffs or specialized skills. Enhancements include the ability to test patients while they are sitting, supine or elevated, and light indicators that confirm the tonometer is positioned properly for measurement. Read more. |
||||||||
|
||||||||
| B+L Licenses Exclusive Rights From Stada & Xbrane for Biosimilar Candidate or Lucentis (Ranibizumab) in US, Canada Bausch + Lomb entered into an exclusive licensing agreement with STADA Arzneimittel AG and its development partner, Xbrane Biopharma AB, a Nordic biosimilar developer, to develop and commercialize a biosimilar candidate to Lucentis (ranibizumab) in the United States and Canada. The companies aim to obtain all currently approved indications for Lucentis in both the United States and Canada. Read more.
|
||||||||
| Luneau’s New Visionix VX65 Digital Phoropter Helps Meet Social Distancing Recommendations Luneau Technology announced the expansion of its Visionix product line with the addition of the VX65 digital phoropter, its next-generation phoropter designed to tackle heavy workloads and meet social distancing requirements in patient care today. The Visionix VX65’s wireless tablet enables operation at a safe patient distance—which could be six feet away, next door or even from a different office location. Learn more. |
||||||||
| Santen Introduces Eco-Friendly Biomass Plastic Eyedrop Bottles Santen Pharmaceutical Co. introduced eyedrop bottles made from environmentally friendly biomass plastic materials. In aiming to contribute to the creation of a low carbon emission recycling-based society, Santen is employing environmental management systems, and working to reduce carbon dioxide emissions, waste production and water usage. It plans to begin introducing the new biomass plastic materials for Timoptol, an ophthalmic solution for treating glaucoma and ocular hypertension. Read more. |
||||||||
| Kala Resubmits NDA for Eysuvis Kala Pharmaceuticals resubmitted its New Drug Application to the FDA for Eysuvis (loteprednol etabonate ophthalmic suspension) 0.25 for the short-term treatment of the signs and symptoms of dry eye disease. Kala, in preparing for a potential U.S. approval and launch by the end of 2020, resubmitted the NDA in response to the FDA’s complete response letter in August 2019 indicating that positive data from an additional clinical trial was needed to demonstrate efficacy and support NDA resubmission. Positive results from STRIDE 3 for signs and symptoms of dry eye disease, along with positive data from the previous clinical trials of Eysuvis, served as the basis for Kala’s NDA resubmission package. As announced in March, the STRIDE 3 Phase III clinical trial met both of its primary symptom endpoints. Read more. |
||||||||
| AI-supported Test Detects Early Signs of Glaucoma Progression A new test can detect glaucoma progression 18 months earlier than the current gold standard method, according to results from a clinical trial. The technology, supported by an artificial intelligence algorithm, could accelerate clinical trials, and eventually may be used in detection and diagnostics, according to a study published in Expert Review of Molecular Diagnostics. The test, called Detection of Apoptosing Retinal Cells (DARC), involves injecting a fluorescent dye into the arm that attaches to retinal cells and illuminates those in the process of apoptosis. The damaged cells appear bright white when viewed in eye exams; the more damaged cells that are detected, the higher the DARC count. One challenge with evaluating eye diseases is that specialists often disagree when viewing the same scans, so researchers incorporated an AI algorithm into their method. Learn more. |
||||||||
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 19 Campus Boulevard, Newtown Square, PA 19073. HOW TO ADVERTISE |