| |
|
| Vol. 1, #01 • Friday, September 18, 2020 |
|
|
|
|
| |
|
Review's Chief Clinical Editor
Paul M. Karpecki, OD, FAAO
Provides you with cutting-edge clinical strategies for optimal management of ocular surface disease and beyond.
|
|
|
|
|
|
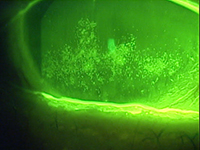 |
| Coalescent punctate keratitis in a patient with advanced dry eye disease. |
As we dive deeply into the latest information and findings about ocular surface disease and, in particular, dry eye disease management, I want to thank Kala Pharmaceuticals for its support of the upcoming Practice Pearls series. Each week you will receive a clinical insight into successfully managing ocular surface disease: optometry’s wheelhouse. By the end of this series, you should feel confident, knowledgeable, and ready to take on this enormous patient population.
So just how big is the dry eye market, and why should we as a profession embrace the management of dry eye disease?
Estimates show that dry eye prevalence ranges anywhere from 5% to 50% based on symptoms alone, and even higher based on signs.1 This tells us that signs and symptoms don’t always correlate to dry eye disease and that the number of patients with either signs or symptoms is staggering.
If we look at two broad based US studies—the Beaver Dam study and the BOSS study (which evaluated dry eye in the children or offspring of the original Beaver Dam participants)—we see a number approaching 14.5% of the US population having dry eye disease. This equates to a staggering 30 million people. Based on the BOSS study, the incidence of DED in younger adults is comparable to that of older adults.2
To put that demographic information in perspective, the prevalence of glaucoma in patients over age 40 in the US is about 2.2 million people.3 Therefore dry eye disease is at least 12 times more common than we originally thought. Especially concerning, based on what I have gleaned from state prescription data, is the fact that that only about 1.7 million of the 30 million people with DED are being actively treated with anything other than artificial tears.
This may be one of the greatest opportunities for the optometric profession we’ve ever experienced. For one thing, DED affects contact lens wear, and we know that more than 7.5 million people drop out every year, costing billions of dollars and millions of unhappy patients. One can argue that spectacle remakes might be largely attributable to dry eye disease. In addition, IOL miscalculations are exceedingly high in patients with DED.4 In one study, 17% of patients with hyperosmolar tears, as measured by TearLab osmolarity, missed their IOL target by more than 1D and as much as 5.5D.4 It has even been suggested that compliance to medications required for blinding conditions like glaucoma is low for reasons including dry, irritated eyes from preservatives such as BAK and pro-inflammatory therapies being applied daily.
Make no mistake about it, dry eye disease is a vision disease; light first hits the eye on the tear film. I have found that the tear film/cornea interface is responsible for about 75% of the refractive error of the eye.
|
|
|
|
|
|
KEY TAKEAWAY: Dry eye disease may be one of the greatest opportunities
the optometric profession has ever experienced.
My aim for this series of clinical pearls focusing on ocular surface disease is to help you better understand, diagnose, target, treat, and manage dry eye patients at an optimal level. My hope is that, upon conclusion of this series, your success in this field will be measurably greater, and the stronger doctor-patient relationships that result will bolster the practice as well.
1. Nelson D, Craig JP, Esen K, et all. TFOS DEWS II Introduction. The Ocular Surface. 2017; 269-75.
2. Paulsen AJ, Cruickshanks KJ, Fischer ME, et al. Dry Eye in the Beaver Dam Offspring Study: Prevalence, Risk Factors, and Health-Related Quality of Life. Am J Ophthalmol. 2014 April;157(4):799-806.
3. Vitale S, Cotch MF, Sperdute RD, et al. Prevalence of visional impairment in the United States. JAMA. 2006;295(18):2158-63.
4. Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. JCRS. 2015 Aug; 41(8):1672-77.
|
|
|
|
| Supported by an independent medical grant from Kala Pharmaceuticals |
|
| |
| |
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 19 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|
|
|
|
|
|
|
|