| |
|
| Vol. 1, #09 • Thursday, November 12, 2020 |
|
|
|
|
| |
|
Review's Chief Clinical Editor
Paul M. Karpecki, OD, FAAO
Provides you with cutting-edge clinical strategies for optimal management of ocular surface disease and beyond.
|
|
|
|
|
|
It is my assumption that most doctors believe the TFOS DEWS II report is complex and requires extensive reading, or perhaps they aren’t even aware of it. Having served on the subcommittee to draft this report, I can tell you that the DEWS II guidance puts forth one of the easiest, most effective, and scientifically sound approaches to DED diagnosis that eye care has seen so far. Here, I will break down the report’s recommended steps to diagnosing DED in your patient.
To begin with, I can save you a lot of reading by simply going through the TFOS DEWS II diagnostic methodology executive summary in Figure 1 below. Click here for a larger version of the Figure.
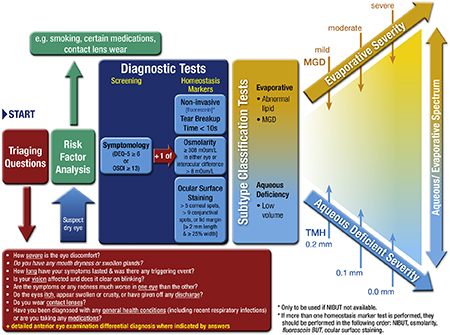 |
Figure 1. TFOS DEWS II Diagnostic Test Battery. Reprinted from Ocul Surf. 2017 Jul;15(3):539-574, Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report, p. 561. © 2017, with permission from Elsevier. |
Steps to DED Diagnosis
Step one in diagnosing DED is to run through a set of patient triaging questions, and we covered five of my favorite questions in last week’s pearl. Next you assess risk factors, which were overviewed in Pearl #4. These include smoking, contact lens wear, certain medications such as antihistamines, etc. This information sets you up for the likelihood of a DED diagnosis and further testing requirements.
Signs and Symptoms
It’s important to note that a diagnosis of dry eye requires some degree of both signs and symptoms. For example, a sign such as superficial punctate keratitis without symptoms may indicate neurotrophic keratitis, while symptoms without signs can point to ocular neuropathic pain or chronic ocular surface pain (COSP).
The recommended approach to assessing symptoms is to use a validated questionnaire such as the DEQ-5 or SPEED. For signs, the DEWS II committee recommended selecting at least one homeostasis test, which may include osmolarity, tear film breakup time (TFBUT), or ocular surface staining. It further recommended noninvasive TFBUT (e.g., devices such as the Oculus Keratograph M5). My suggestion would be to use at least two of the three homeostasis diagnostic options.
DED Subtype
Armed with positive symptoms and signs, the next step is to determine the DED subtype. The two subtypes are: evaporative dry eye (EDED) caused by meibomian gland dysfunction; and aqueous deficient DED (e.g., keratoconjunctivitis sicca [KCS] or Sjögren’s syndrome KCS).
EDED is best determined by expressing the meibomian glands: A clear olive oil-like expression using minimal pressure is normal; on the other hand, turbid, discolored, gelatinous, paste-like expression, and non-expression are abnormal signs. To determine if a patient has the aqueous deficient subtype, observing the tear meniscus height is key. Less than 0.2mm is considered abnormal and indicative of aqueous deficient DED. But rather than measuring, if you simply get comfortable with what a normal tear meniscus height looks like, you’ll quickly recognize one that is deficient.
Finally, keep in mind that many patients can have some degree of concomitant evaporative and aqueous deficient DED, known as mixed forms. Although inflammation is the one consistent finding in both subtypes, treatments will vary based on which type you are managing. We’ll discuss treatment in future clinical pearls.
|
|
|
|
KEY TAKEAWAY: The TFOS DEWS II report puts forth one of the easiest, most effective, and scientifically sound approaches to DED diagnosis that eye care has seen so far.
|
|
|
|
| Supported by an independent medical grant from Kala Pharmaceuticals |
|
| |
| |
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 19 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|
|
|
|
|
|
|
|