| Access sessions, exhibit hall and special events through the Academy event planner. |
For more than 70 years, the Academy has encouraged optometry students to pursue careers in research and education with the Ezell Fellowship. More than 400 students have received the honor, and this year three more join their ranks: Danielle M. Robertson, OD, PhD, FAAO, Suresh Viswanathan, BOpt, MS, PhD, FAAO, FARVO, and William Tuten, OD PhD.
This year’s Ezell Fellows Presents lecture, taking place October 14, 5-7pm Eastern Time, will tackle an ever-expanding topic: clinical imaging. The field has witnessed unprecedented advances, allowing researchers detailed visualization of ocular structures like never before.
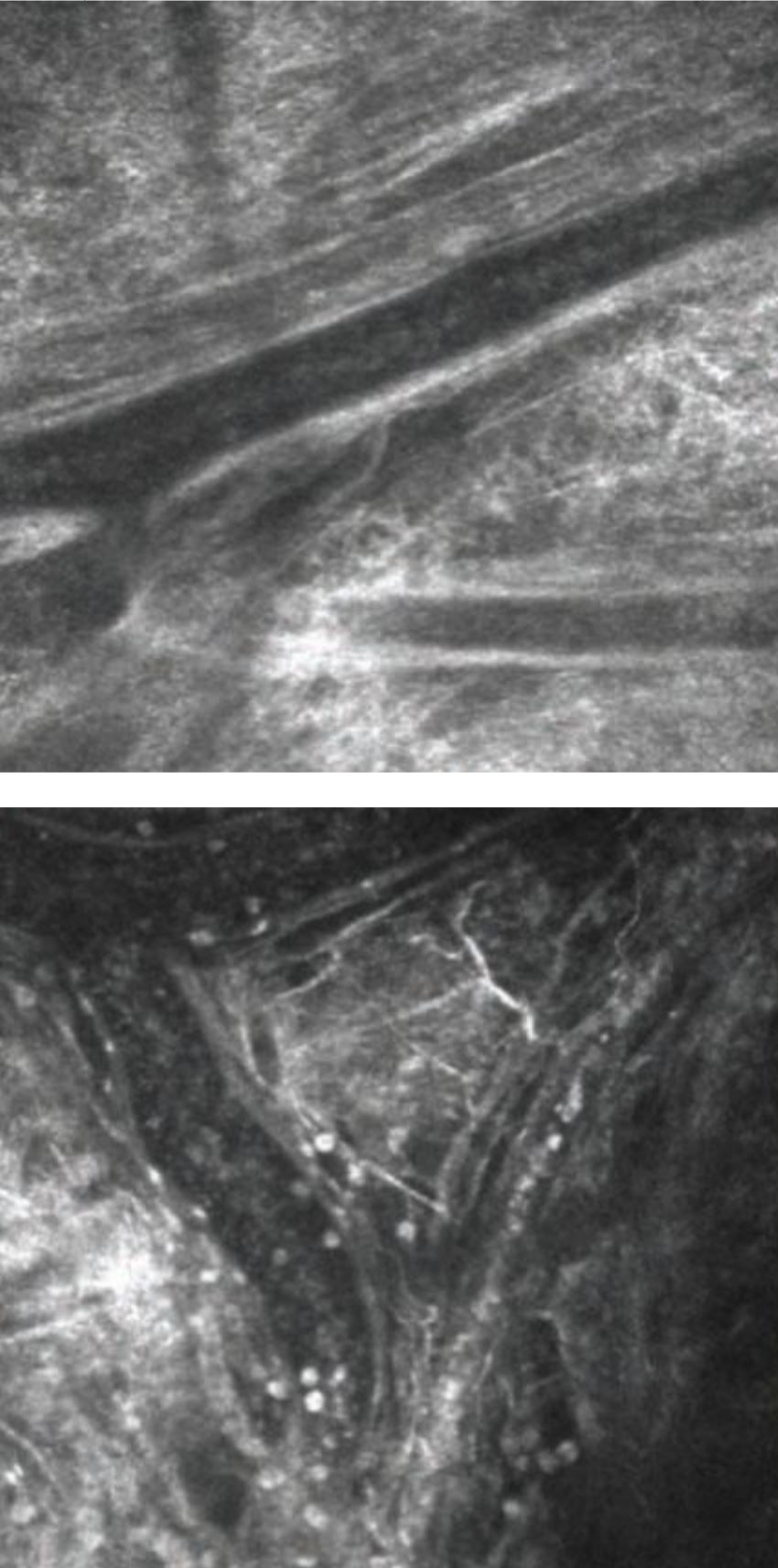 |
| In vivo imaging of conjunctival blood vessels before (left) and after (right) allergen challenge. White cells are clearly visible following challenge, and some of these can be see migrating out of vessels into extravascular space. Photo: Mark B. Abelson, MD, CM. Click image to enlarge. |
Anterior Structure Layer By Layer
Moderated by William Ngo, OD, PhD, FAAO, the session will kick off with a comprehensive look at in vivo corneal imaging with Dr. Robertson. In the past, imaging with white light confocal microscopy and confocal microscopy through-focusing was mainly used for four clinical presentations: keratorefractive surgery, infectious disease, wound healing and corneal dystrophies/degenerations. While incredibly useful, the technology wasn’t widely used in day-to-day practice.Now, researchers and clinicians have laser scanning confocal microscopy, which provides precise imaging, even on a cellular level. Corneal nerves, corneal thickness, fibrosis and the ocular adnexa are now visible using this technology.
Likewise, OCT may have started out as an imaging tool for the posterior segment, but researchers are quickly understanding its ever-expanding utility for corneal health. Corneal thickness measures and epithelial thickness mapping are becoming increasingly important for comprehensive corneal assessment. Even OCT angiography is showing promise as an anterior segment imaging tool, according to Dr. Robertson.
The corneal imaging session will wrap up with a look at future technology, including second harmonic generation microscopy, fluorescence-lifetime imaging microscopy, cellular autofluorescence and brillouin scattering—all of which will help researchers better understand the intricacies of corneal structure and dysfunction.
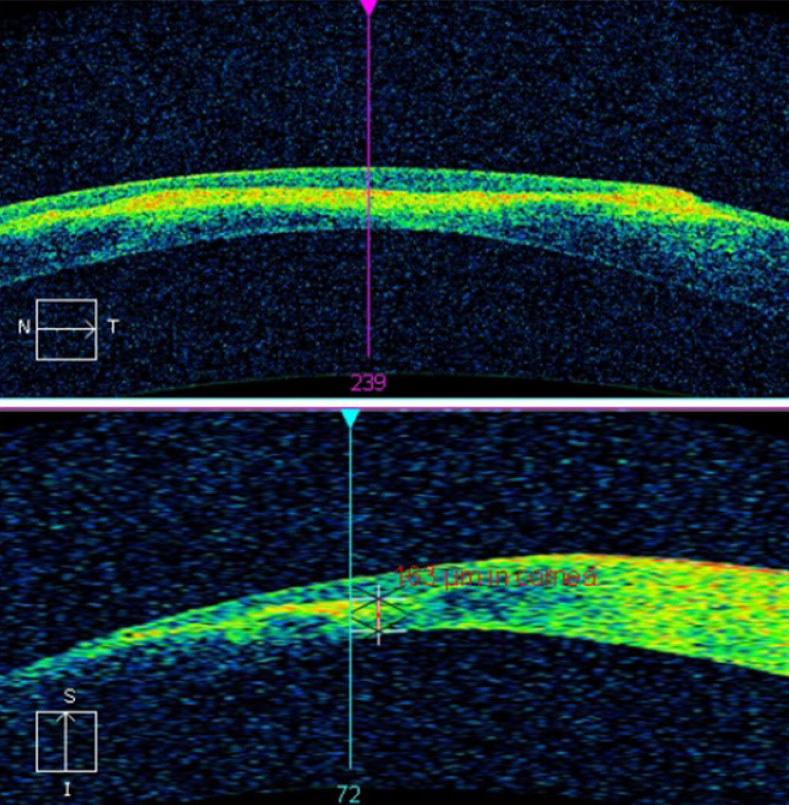 |
| This AS-OCT scan of a 28-year-old Asian patient with advanced keratoconus and moderate-to-severe pain demonstrates intact endothelial and posterior stromal layers while showing increased reflectivity associated with stromal scarring. In this case, AS-OCT confirmed an intact endothelium and Descemet’s membrane. As an added advantage, corneal thickness was measured accurately at the thinnest location using the caliper tool, thereby providing a reliable baseline for follow-up comparison. In light of the anatomical state of the cornea, the patient’s symptoms were attributed to epithelial disruption overlying the apex of corneal steepening. Photo: Carolyn Majcher, OD. Click image to enlarge. |
A Better Posterior View
Moving to the posterior segment, Dr. Viswanathan will turn everyone’s attention back to OCT and its utility in tracking changes in optic nerve parameters due to repeated intraocular pressure (IOP) spikes. His lab’s current research is looking beyond IOP measurements to track the risk of glaucoma progression using OCT retinal nerve fiber layer thickness, Bruch’s membrane opening minimum rim width and anterior lamina cribrosa surface depth.
These OCT measures may help his team see the momentary structural deformation of the optic nerve as a response to a patient’s day-to-day IOP spikes—possibly revealing new risk factors for progression, he suggests.
To wrap up the session, Dr. Tuten will discuss the adaptive optics (AO) scanning laser ophthalmoscope, a new tool that provides noninvasive imaging of the photoreceptor structure in patients with retinal degeneration. Research shows changes to the outer retinal structure on a cellular level, although conventional clinical devices lack the resolution and precision necessary to characterize the visual function on a commensurate scale, according to Dr. Tuten.
However, AO microperimetry is changing that. Dr. Tuten will give attendees a glimpse into the principles of the technology and will then share its utility in two clinical trials. The new imaging technology has proven invaluable for detecting changes in eyes with macular telangiectasia type 2 and choroideremia. Using the promising trial data, Dr. Tuten will help attendees understand the implications of the newfound ability to measure visual function at the cellular level. AO microperimetry may prove integral to clinical studies that evaluate how the diseased retina responds, on a cellular level, to experimental interventions—another significant breakthrough for a field already realizing gene therapies.
