| Access sessions, exhibit hall and special events through the Academy event planner. |
If you’re looking to differentiate the glaucoma care you provide, then tomorrow afternoon’s session, “Patient Centric Approach to Glaucoma,” will leave with a better understanding of how to plan a care regimen around each patient, not just their condition. The event takes place October 8, 2-3pm Eastern Time.
“In glaucoma care, clinicians often gauge success based solely on lowering intraocular pressure (IOP). However, both the disease and the treatment itself can have a profound impact on our patients’ quality of life,” says Andrew Rixon, OD, FAAO, one of the facilitators. “This course examines the impact of glaucoma on our patients and society, from a public health, clinical and patient perspective in order to maximize our awareness of the necessity of providing more enlightened care beyond simply lowering IOP.”
The team of Gregory Wolfe, OD, MPH, FAAO, FNAP, Andrew Sacco, OD, FAAO, Karen Squier, OD, MS, FAAO, and Dr. Rixon will open the presentation with a conversation about the continuum of symptoms that follow the progression of glaucoma, ranging from normal to blindness. They’ll then follow-up with some of the factors affected by the disease, including cost and quantity and qualify of life, and the role eye care providers can play in managing each.
The remainder of the lecture is broken up into three parts, the first covering glaucoma from a clinical standpoint. Dr. Sacco will take the lead with a discussion on the resources glaucoma patients seek out for educational purposes, namely, internet sites, print materials, advocacy groups and professional associations. These patients usually question the symptoms of glaucoma first in an attempt to anticipate what their experience will be like. Much to their dismay, most resources will point toward a lack of symptoms until the disease has progressed further along. They’ll expect tunnel vision, loss of side vision and blind spots, but will more than likely only experience missing spots, empty vision, smudges, blur, loss of light or no symptoms at all earlier in the disease process. They may also suffer from contrast or color sensitivity, high spatial frequency loss or facial recognition difficulty.
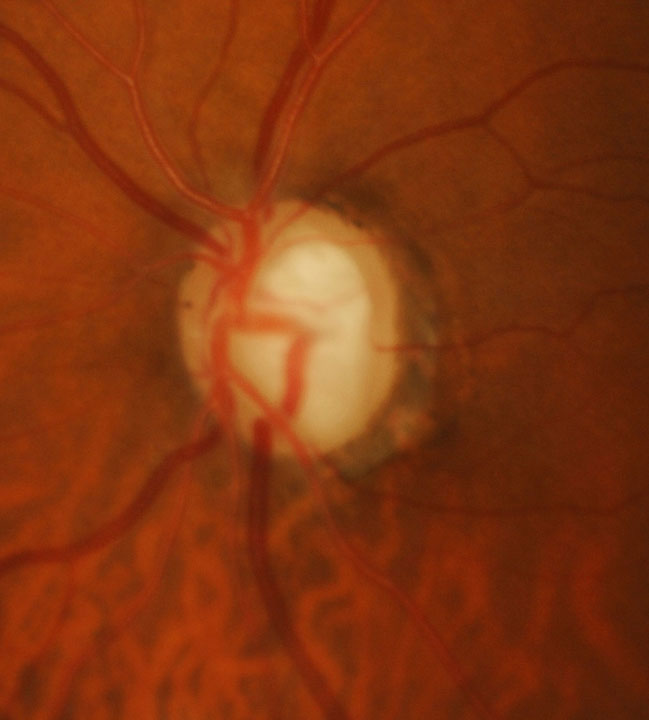 |
| This patient has advanced disease OS. Late-stage glaucoma is associated with substantially worse quality of life. Click image to enlarge. Photo: Andrew Rixon, OD |
The next segment introduces barriers to success and potential solutions. Dr. Rixon will offer a few ways eye care providers should gauge success with glaucoma, rather than focusing solely on IOP reduction. These include slowing the rate of disease progression, focusing on patient-centered outcomes and monitoring results for improvement. Unfortunately, standard automated perimetry does not come without flaws. These include but are not limited to the variability in performance and results, high volume of tests required to detect change, baseline readings that do not tell the whole story, poor sampling capability, need for a highly trained perimetrist and lack of machine portability.
This combined with the lack of compliance on the patient’s part and the lack of acknowledgement on the eye care provider’s part could prove fatal. Solutions include comprehensive education and honest communication with open-ended questions in a non-judgmental environment where the provider sets the tone and involves the patient in decision-making.
Last but not least is a section on vision rehabilitation for glaucoma. Dr. Squier covers when to think about referring glaucoma patients for low vision services, taking different factors into consideration, such as visual acuity, contrast loss, field loss, scotomas, reading trouble, mobility complaints, driving difficulty and facial recognition. She also includes what low vision options are available and which are best suited for which patients.
By altering eye care providers’ perception of and shedding light on what glaucoma patients experience, Dr. Rixon hopes attendees will be able to engage in patient-centered communication, promoting more successful outcomes. “Improving physician and patient awareness of the burdens of glaucoma will help shift everyone’s focus, driving us toward more meaningfully capturing the totality of the disease state and preventing functional vision loss,” he says.
