Attendees can learn how to approach demyelinating disease and neurodegenerative disorders from all angles by attending this year’s “Larry Gray Memorial Symposium on Neuro-Ophthalmic Disorders: Optic Neuritis, Neuro-immunity and Demyelinating Disease.” The session, taking place October 12, 9-11pm Eastern Time, will combine the perspectives of an optometrist, a neuro-ophthalmologist and a neuro-immunologist to demonstrate how each specialty can use its strengths to work together for the best interest of the patient. Leonard Messner, OD, FAAO, Reis Longmuri, MD, and Francesca Bagnato, MD, PhD, will discuss the clinical ocular presentation and exam findings for different types of optic neuritis and optic neuropathy cases.
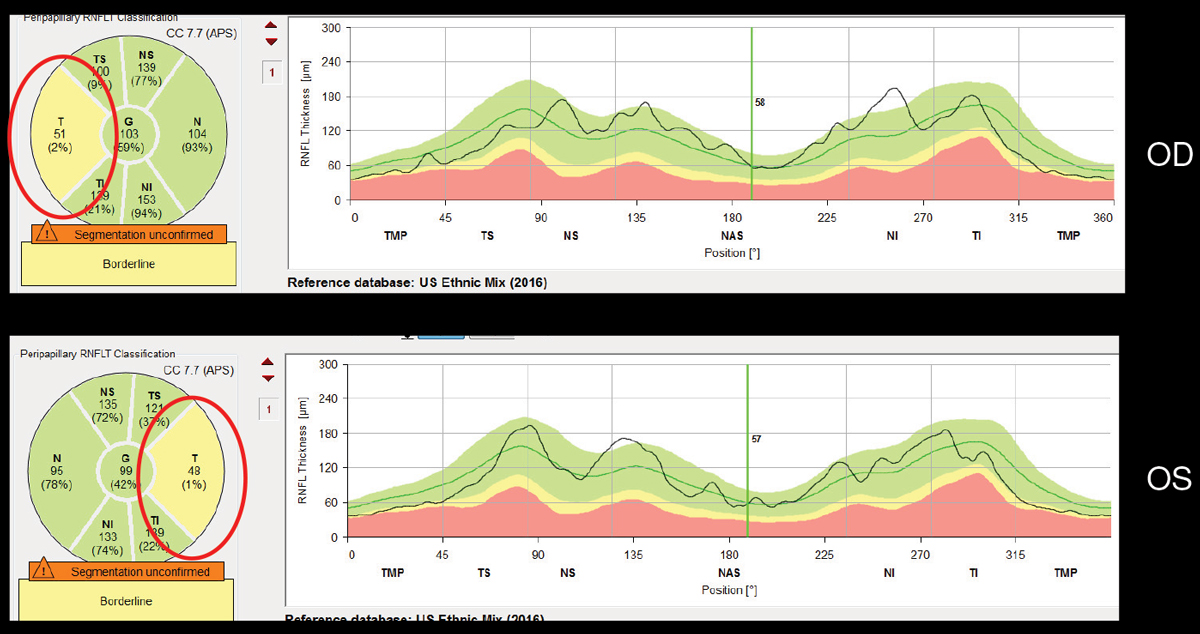 |
| In MS, RNFL thinning tends to be greatest temporally and inferior temporally. |
“Other specialists who treat patients with demyelinating disease can work closely with eye care professionals to get a better sense of how adequately a patient’s disease process is being managed,” says Kelly Malloy, OD, FAAO, chair of the symposium. “Eye care professionals can also help with proper diagnosis and management by recognizing features of optic neuritis that are less likely associated with multiple sclerosis (MS).”
The session will open with a review of using OCT findings in not only monitoring progression of demyelinating disease, but also in assessing for the presence and progression of other neurodegenerative diseases as well, such as Parkinson’s disease, Alzheimer’s disease and traumatic brain injury. “Optometrists can play a helpful role in the management of patients with demyelinating disease in not only acute, but also chronic cases, especially through the use of OCT,” Dr. Malloy says.
Dr. Messner will present how OCT thinning can occur in demyelinating disease, even without an acute event of optic neuritis. In MS, the degree of retinal nerve fiber layer (RNFL) thinning does correlate with patient quality of life. In addition, OCT ganglion cell/inner plexiform thinning correlates with new MS lesions and duration of disease. Ganglion cell/ inner plexiform layer (GPIPL) thickness is a stronger marker of visual impairment as compared with RNFL thickness.
The speakers will discuss how various types of demyelinating disease have different pathologic mechanisms, and therefore, different diagnostic testing protocols and treatment options. Also, attendees learn the importance of understanding other non-demyelinating causes of optic neuritis, such as infectious, metabolic and cancer-related mechanisms. Dr. Bagnato will present on the clinical manifestations of optic neuritis as well as its many differential diagnoses, from more frequently to less frequently encountered.
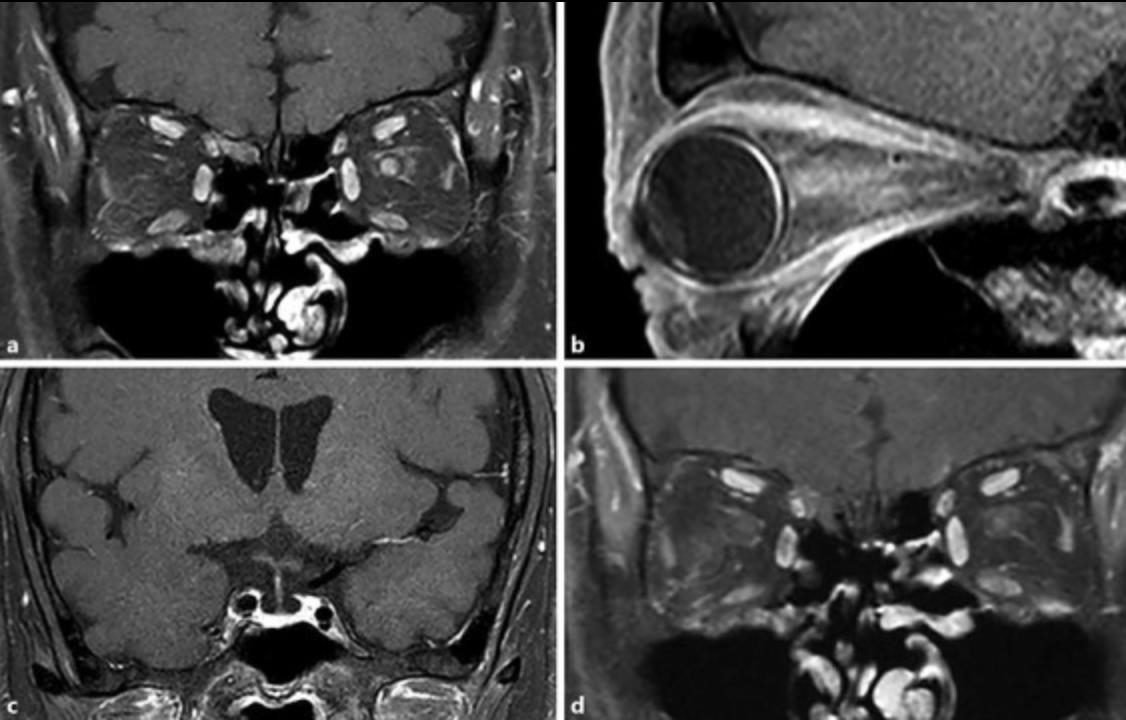 |
| The appearance of optic neuritis on MRI. |
“The expertise of a neuro-ophthalmologist can help to better determine how the clinical presentation may point to a particular etiology and initiate the necessary work-up, whereas the expertise of a neuro-immunologist can help fine tune the detailed work-up as needed and recommend the most up-to-date treatment options in the rapidly changing world of neuro-immunology,” Dr. Malloy notes.
“Attendees will learn that optometrists must work closely with other health care providers to determine the proper etiology and treatment for each individual optic neuritis,” Dr. Malloy says. “We must not assume that every optic neuritis is secondary to MS.”
Dr. Malloy also notes that getting the appropriate work-up, which may include neuro-imaging, lab testing and CSF analysis for oligoclonal bands can be critical to proper patient management. “That inter-professional collaboration does not stop once the diagnosis and treatment are established,” she emphasizes. “Through OCT, eye care professionals can help to assess progression of the underlying disease process even in the absence of another acute event.”
