This year’s annual meeting has a few special virtual sessions in store for attendees, including tonight’s Anterior Segment Section Symposium, “Ocular Surface Reconstruction: Putting the Pieces Back Together,” moderated by Jacob Lang, OD, FAAO, taking place October 13, 9-11pm Eastern Time. The symposium is broken up into multiple parts, each of which targets a different advancement in reconstructive treatment.
“From mild to severe ocular surface disease, management of the ocular surface is critical for ocular health and vision,” Dr. Lang says. “These tissues are the ‘first line’ between our eyes and the external world and are, therefore, the ‘gateway’ for many things, including light.”
Joseph Shovlin, OD, FAAO, will open the session with a discussion of amniotic membrane transplantation (AMT). The amniotic membrane, an avascular fetal membrane that lies deep in the chorion and is harvested from placental tissue obtained during cesarean sections, inhibits fibroblasts and cell death, reduces inflammation and pain, protects the ocular surface and enhances epithelial adhesion and migration by promoting stem cell expansion.
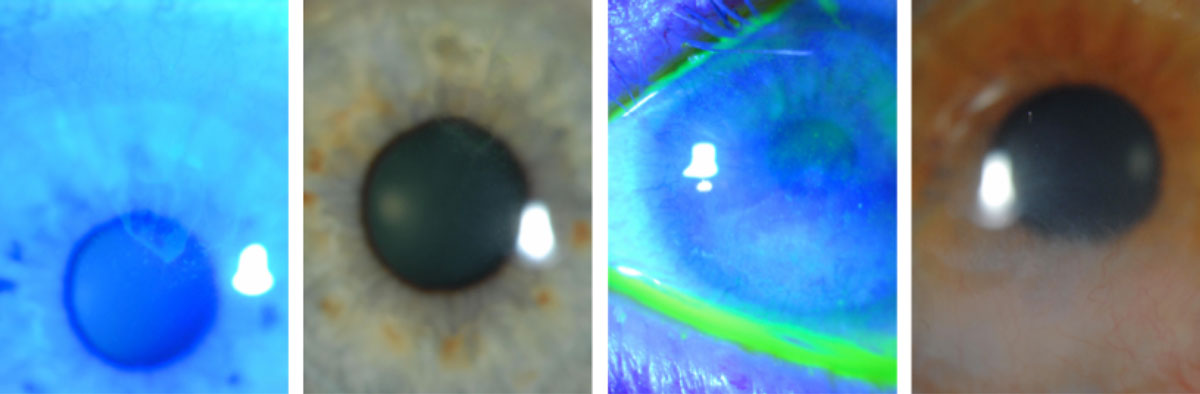 |
| LSCD in two different contact lens wearers shows a typical dull haze/irregular reflex with a “whorl,” conjunctivalized cornea (white light) and a late, stippled fluorescein effect (cobalt filter). Click image to enlarge. |
Transplanted membranes are either cryopreserved or dehydrated. Dr. Shovlin will review studies comparing the two, explaining how cryopreserved tissue retains the native architecture of the amniotic membrane and umbilical cord and maintains the biological signals of both.
AMT indications include corneal defects, delayed corneal healing, corneal dystrophies and degenerations and ocular surface damage. A transplant is medically necessary in the case of a persistent epithelial defect (PED), uncontrolled inflammation, delayed healing and failed therapy. Dr. Shovlin will show how a 67-year-old recurrent herpes simplex keratitis and dry eye patient found success with AMT. Studies support this result, reporting that cryopreserved amniotic membranes encourage corneal nerve regeneration and ocular surface recovery and reduce clinical signs and symptoms in dry eye patients.
Moving on from AMT, Dr. Shovlin will focus on limbal stem cell deficiency (LSCD) in contact lens wear. LSCD is caused by any process that harms the stem cell environment and diminishes the number and/or function of stem cells and may have inflammatory, traumatic, infectious, congenital, neoplastic or iatrogenic roots. It may present with reduced acuity, photophobia, pain, irritation and/or tearing. Dr. Shovlin will highlight what to look for on clinical examination and diagnostic testing.
Whether a specific case of LSCD is partial or complete, or unilateral or bilateral dictates the appropriate treatment route. Management techniques include surface restoration, stem cell transplantation, keratoprosthesis and serum tears upon early detection for the best results.
Dr. Shovlin will then hand the microphone off to Albert Cheung, MD, who will present on ocular surface stem cell transplantation. Dr. Cheung recommends eye care providers stay away from keratoplasties for ocular surface disease secondary to conjunctival or LSCD, as this procedure eventually fails. This sets candidates up for an even worse transplantation prognosis. Fortunately, patients have several autograft and allograft transplantation options available to them.
As far as the preoperative workup and postoperative management go, patients must undergo appropriate testing and monitoring. Dr. Cheung will pinpoint what to keep an eye out for and how to proceed accordingly, especially in the case of rejection, failure, PEDs, glaucoma or infectious keratitis.
Shifting the spotlight, Dr. Cheung will cover neurotrophic keratitis, a degenerative disease that may lead to temporary or permanent visual dysfunction if left untreated. He’ll touch on its effects, such as altered corneal sensation, loss/imbalance of trophic factors and altered lacrimal function, and its causes. These include infectious vs. non-infectious, systemic disease, iatrogenic, medication-induced, congenital disease and trigeminal nerve palsy. Depending on a patient’s signs and symptoms, neurotrophic keratitis can be classified into three stages: mild, moderate or severe. Treatment focuses on optimizing the ocular surface, treating eyelid abnormalities, sheltering the ocular surface microenvironment and directly treating the ocular surface.
Guillermo Amescua, MD, will then move on to keratoprosthesis and mucous membrane grafting, from indications and procedural overviews to complications and management to outcomes and areas for improvement.
Karen Carrasquillo, OD, PhD, FAAO, FSLS, FBCLA, will close the symposium with a discussion on treatment with the PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) device. Dr. Carrasquillo will touch on the trifecta of therapeutic benefits it offers: visual rehabilitation, improved comfort and ocular surface support. She’ll then go over several case examples that illustrate the restorative nature of PROSE devices, including a 23-year-old patient with type one diabetes and PEDs secondary to neurotrophic keratopathy, a 60-year-old pellucid marginal degeneration patient, a 66-year-old graft-vs.-host disease patient with chronic PEDs that resulted in bilateral corneal melting and a 44-year-old Stevens-Johnson syndrome patient with LSCD. All underwent several unsuccessful treatments before achieving better results with a PROSE device.
“This lecture is a great panel-based discussion of the many techniques, technologies, procedures and surgeries we have at our disposal to help rehabilitate the ocular surface from injury, disease or other conditions,” says Dr. Lang.
