 |
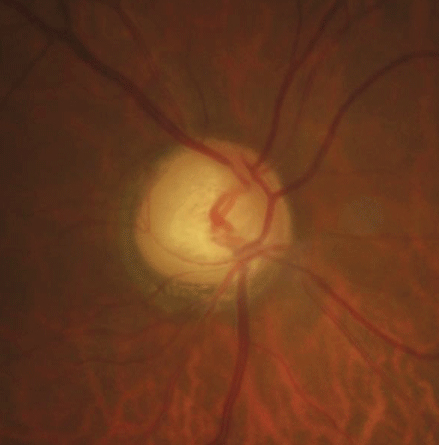
| A simple-to-obtain fundus image can reveal glaucomatous thinning, as seen here. Photo: Justin Cole, OD, and Jarett Mazzarella, OD |
As the only modifiable risk factor for glaucoma, intraocular pressure (IOP) has an outsized influence in glaucoma care. Many clinicians rely on IOP reduction to determine whether patients are achieving therapeutic success. However, speakers in Thursday afternoon’s “Rapid Fire: A Patient Centric Approach to Glaucoma” session challenged optometrists to consider additional factors that may yield more meaningful glaucoma information.
Prioritize Vision, Not IOP
“We become fixated on IOP as our gold standard as we talk about treatment for glaucoma,” said Gregory Wolfe, OD, MPH, FAAO, associate professor and co-director of the Center for Eye and Health Outcomes at Southern College of Optometry. “Of course, we look at visual fields and functional outcomes to see if they are progressively losing vision. But we use that target IOP as a quick measure of” treating efficacy. “Sometimes, we get laser-focused on IOP and we forget that IOP is connected to a human being that’s living in the real world and has real-life problems beyond just the fact that they have elevated IOP or glaucoma.”
Dr. Wolfe cited the cost of glaucomatous visual impairment to the economy—about $5.8 billion, according to a July 2013 NORC/University of Chicago study. Glaucoma and diseases of the optic nerve cost more than $2,000 per person, according to a 2006 study (Lee PP, et al.) in Archives of Ophthalmology. Yet, low-vision rehabilitation services don’t occur in a meaningful way until patients get to the later stages of glaucoma, Dr. Wolfe said. He suggested those services need to occur sooner in the life course of disease as a way to provide more holistic glaucoma care. And he stressed the importance of looking at the environmental and social conditions in which glaucoma patients’ live because those factors heavily influence health outcomes.
Problems With Perimetry
|
In 1948, the World Health Organization adopted the statement that “health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Dr. Wolfe suggested that, similarly for the glaucoma patient, the goal is to maintain vision and lead a healthy, meaningful life.
While some eye care practices are embracing screenings to identify early disease, he said optometry has an opportunity to practice primary preventive care to address the risk factors that lead to disease. In looking at such factors, practitioners must move beyond the well-known indicators of age, race, IOP and central corneal thickness as possible factors, to consider others such as obstructive sleep apnea, obesity and nutrition. Furthermore, Dr. Wolfe discussed measures assessing patient quality of life.
In Their Own Words
Andrew Sacco, OD, FAAO, of Vestal, NY, gave examples of outdated information that glaucoma patients may find online about visual defects and underscored the importance of controlling how patients learn about their condition.
He highlighted studies revealing that patient descriptions about visual defects aren’t necessarily the cliché “tunnel vision,” but can reference glare and jarring changes to lighting conditions. In some papers (Crabb DP, et al., 2013; Fujitani K, et al., 2017), glaucoma patients have described “black and blurred tunnels,” “black parts,” “border parts” and “missing parts.” They also have expressed difficulties with contrast sensitivity, color, high spatial frequency loss and facial recognition.
“I think what’s important is looking at what a patient tells you in their own words and asking them” about it, Dr. Sacco said.
Toward that end, researchers have begun using more patient-reported outcome measures (PROMs) in clinical trials. PROMs are measurements of varying complexity to gather information from the patient’s point of view. Although they can be challenging to administer and interpret, Dr. Sacco would like to see increased use of PROMs earlier on in research and in clinical practice.
Does my patient need low vision rehabilitation?American Academy of Ophthalmology recommendations:
American Glaucoma Society says only 22% follow these guidelines for referral and, of that 22%, only 38% refer specifically for low vision rehabilitation |
“The more we can take a patient-centric approach, and the more we can ask our patients how they’re doing and how they’re handling the treatment, the better we’re going to handle the disease and our patients, and it’s not all going to be about controlling the pressure in the eye,” Dr. Sacco said.
Beyond Static Pressure Readings
Exploring the dangers of using IOP measurements to gauge treatment success, Andrew Rixon, OD, FAAO, resident faculty at Southern College of Optometry, pointed out that although lowering IOP is the only intervention for glaucoma, some patients continue to lose vision regardless of their ability to capture target pressure. “There’s this peril of using a static pressure that we capture once every three months to gauge success,” Dr. Rixon said.
He noted that no major glaucoma studies he was aware of have addressed ideal pressures for glaucoma patients or groups. And just decreasing IOP isn’t enough of a benchmark, the reduction has to be based on trend analysis from visual fields and structural analysis, he added. Furthermore, Dr. Rixon said, use of targets hasn’t been proven to make a meaningful difference in glaucoma management because clinicians aren’t able to effectively capture IOP beyond office hours.
Yet, the tendency to focus heavily on pressure readings can lead to “IOP obsession,” Dr. Rixon said. “The patient comes in, they want the [target] number that you told them. You want the number. Meanwhile, if they don’t meet the number, sometimes they’re doing great. If they meet the number, sometimes they’re actually doing horribly. So we have to reframe the conversation with our patients.”
New Evaluation & Detection Strategies
The one reliable way to know that treatment is working is to document a lack of disease progression, Dr. Rixon said. New strategies to evaluate successful glaucoma management and predict future rates of progression are focusing on patient-centered outcomes, and visual and healthcare quality of life, which require sufficient testing to make the information valuable, he added.
When should I consider a referral?
|
In addition, limitations of current detection strategies, perimetry in particular, have led to the birth of neurodiagnostic devices, some combined with virtual reality (VR) such as the nGoggle, to reduce subjectivity and increase portability in glaucoma evaluations. Such devices analyze electrical activity and information in the brain, enabling researchers to capture visual field information based on visual stimuli that are presented. And new software is being developed to better assess right and left eye movements in a binocular environment unlike visual fields, which operate in a monocular environment, while VR is being used to more reliably predict falls in glaucoma patients.
Moreover, Dr. Rixon stressed the importance of doctor-patient communication for medication adherence, as studies have shown that improved communication contributes to better adherence. And Karen Squier, OD, MS, FAAO, an associate professor at Southern College of Optometry, rounded out the discussion with practical ways to apply vision rehabilitation to glaucoma patients.
Dr. Rixon summed up the theme of the session best when he told attendees: “I challenge everyone to start managing a disease, rather than three seconds of IOP that you’re getting every three months.”
