 |
Q: I had a patient recently who came in complaining of an itchy eye. She had an eye exam eight months ago. How far should I go with the workup?
A: Though this patient was recently seen by another eye practice, she is new to you, warranting a full new patient examination, according to David J. Baptiste, OD, an optometrist working in Fort Worth, Texas. This consists of a comprehensive workup, including vitals (i.e., blood pressure), retinal photos and a visual field screening test. The patient reported self-medicating with over-the-counter allergy remedies to relieve the itching, which had persisted for more than six months in her left eye. She was not wearing any refractive correction other than over-the-counter reading glasses.
While the Texas allergy season lasts the whole year round, Dr. Baptiste notes, the fact that the itching was unilateral is atypical for an allergic eye presentation. The patient’s unaided VA was 20/20 OU. Additionally, the external examination revealed swollen upper and lower lid margins as well as crusting at the base of the patient’s lashes—leading to the diagnosis of blepharitis.
Review of the entrance test results from the screening visual field testing revealed a mild defect in the lower left visual field. While possibly a false positive, it is not good practice to ignore such a seemingly mild finding. For this reason, a second test was administered 30 minutes later to confirm results, according to Dr. Baptiste. The re-test revealed a similar but more pronounced field defect. When questioned, the patient admitted to some visual impairment while driving. She specifically reported that she had difficulty merging into traffic and not always seeing cars on her left side as she entered the roadway. Based on these warning signs, Dr. Baptiste recommended the patient see a neurologist immediately. He went a step further and called to make the appointment, not leaving the referral to chance.
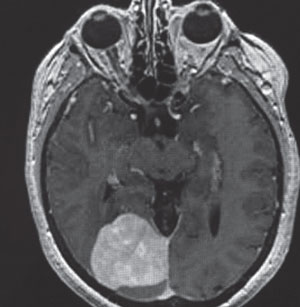 | |
| A scan of the patient’s meningioma. Photo: Anthony Lee, MD. |
The neurologist she saw ordered an MRI and identified the tumor as a meningioma attached to the falx cerebri and tentorium cerebelli, roughly 4cm in diameter and pressing on the occipital lobe. Though the tumor was benign, meningioma growth can impact speech, motor skills and ultimately, breathing and heart function, depending on their location. The neurologist told Dr. Baptiste that he believed the tumor had been growing for roughly 15 to 20 years, and would have been inoperable within another five to 10 years.
The patient was scheduled for surgery three weeks after the initial eye examination and, ultimately, the procedure was successful. The patient recovered and returned to work six weeks later. No tumor regrowth was found at the one-year follow-up appointment. The patient remains extremely grateful for Dr. Baptiste’s life-saving catch.
So what can we, as practitioners, learn from this case? First, even if a patient recently saw another doctor, the moment she steps through your door you are now responsible for her vision and visual health. Be thorough, and don’t exhibit the mentality that “they must have done that at the other office so I don’t need to.” Assumptions like this can lead to disaster.
Second, while it is not practical to order an MRI every time a patient misses a point or two on a visual field, if there are a cluster of points missed, either on an FDT or formal automated field, it should be repeated. If the defect persists, a consult with a neurologist should be considered.
Third, do not leave it up to the patient to make the appointment, as many ultimately will. Direct your staff to make the appointment and document the time and date of the exam. If the patient fails to make the visit, any subsequent issues are on her.
