New research from the National Eye Institute (NEI) suggests the retina-specific immune cells that are causally involved in autoimmune uveitis have their beginnings in the gut.
“Understanding what spurs autoimmune uveitis is fundamental to the development of safer long-term therapies and possibly even strategies for preventing it,” Reiko Horai, PhD, a staff scientist at NEI and a lead author of the study, says in an NEI press release.
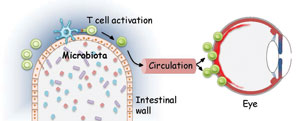 | |
| Immune cells activated in the gut migrate to the eye, where they cause the inflammatory response associated with autoimmune uveitis. Image: National Eye Institute, part of NIH. |
Because the eye is an immune-privileged site, researchers have struggled to understand how the immune cells become activated while their antigens are separated behind blood-tissue barriers. The new study found the cells receive the activation signal in the gut, an action that precedes the clinical onset of the disease.
Once they discovered the location of the immune cell activation, the investigators speculated that bacteria in the gut produce a molecule similar to the retinal antigens, thus prompting the immune cells to activate and seek the proteins in the eye. To support this theory, they activated retina-specific immune cells by exposing them to bacterial proteins extracted from mouse intestines. When they injected the activated cells into normal mice, they developed uveitis.
While the researchers note the findings have no impact on patient care yet, they hope it will help scientists one day identify the bacteria specifically involved in promoting autoimmune uveitis, possibly leading to targeted therapy options.
Horai R, Zárate-Bladés CR, Dillenburg-Pilla P, et al. Microbiota-Dependent Activation of an Autoreactive T Cell Receptor Provokes Autoimmunity in an Immunologically Privileged Site. Immunity. 2015;43:343-53.
