Your Diagnosis
A 27-year-old black man presented for an eye examination following a blunt ocular trauma. He was elbowed in the right eye during a basketball game. His previous systemic history and ocular history were noncontributory.
Diagnostic Data
His best-corrected visual acuity was 20/40 O.D. and 20/20 O.S. at distance and near. External examination was normal, and there was no evidence of afferent pupillary defect. Anterior segment structures were normal. Goldmann intraocular pressures measured 15mm Hg in both eyes.
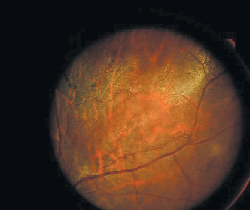
The pertinent fundus findings are demonstrated in the photograph.
The patient"s left eye had this appearance.
How would you approach this case? Does this patient require additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
The diagnosis in this case is commotio retinae O.D.
Additional testing may include close inspection of the orbit for emphysema or crepitus, X- ray or CT scan to rule out fracture, close inspection of anterior chamber for inflammation or hyphema, close inspection of the posterior peripheral fundus to rule out retinal breaks or tears, and photodocumentation. Gonioscopy is not advisable immediately following blunt injuries. Gonioscopy should be performed following the episode"s resolution to assess the angle for damage. This patient will need to be regularly monitored for glaucoma for the rest of his life.
Commotio retinae (Berlin"s edema) occurs as a result of contrecoup injury. Relatively well-defined areas of retinal opacification develop shortly after the injury. Experimental evidence and clinical observation suggest the retinal changes are secondary to deep sensory retinal edema.
Histologically, receptors and cell bodies in the outer nuclear layer are damaged early. Retinal pigment epithelium then phagocytoses outer segment material. Retinal pigment epithelium next undergoes hyperplasia and may migrate into the retina, depending on the severity of the initial trauma.
The process may resolve completely without sequelae, or damage to the photoreceptors may cause permanent visual loss. Cystoid macular degeneration with cyst and hole formation may occur months or years later. Microcysts may break down, resulting in posterior polar retinoschisis (macular cyst) or the development of a macular hole (lamellar hole). If a posterior vitreous detachment ensues, epiretinal membrane may form and result in retinal wrinkling and reduced acuity. Any time the retina is exposed to traction, hole formation is a possibility.

