A 35-year-old white male presented with blurred vision in both eyes for the past three to four weeks. He said that the vision loss occurred gradually. He also began to experience flashes and floaters in both eyes around the same time.

He initially presented to another vision clinic at which the doctor advised him to see a retinal specialist.
On examination, best-corrected visual acuity measured 20/25 O.D. and 20/30 O.S. Confrontation visual fields were full to careful finger counting O.U., and his pupils were equally round and reactive with no afferent pupillary defect. Ocular motility testing was normal.
The anterior segment exam was unremarkable. IOP measured 14mm Hg O.U.
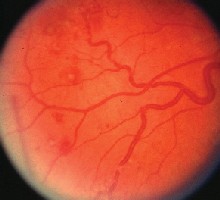
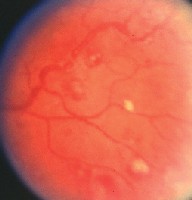
The findings from the dilated fundus exam are shown in figures 1 to 4.
1, 2. The dilated fundus exam (O.D. left, O.S. right) showed these ominous retinal changes in a 35-year-old male patient.
Take the Retina Quiz
1. How would you best describe the optic nerves?
a. Normal.
b. Papilledema.
c. Pseudopapilledema.
d. Papillitis.
2. What is the most significant finding along the arcades?
a. Dilated retinal veins.
b. Retinal hemorrhages.
c. Cotton-wool spots.
d. Roth spots.
3. What test would be most helpful in diagnosing the patient?
a. Magnetic resonance imaging.
b. Complete blood count (CBC) with differential.
c. Fasting blood sugar.
d. Fluorescein angiogram.
4. What is the likely diagnosis?
a. Idiopathic intracranial hypertension (pseudotumor cerebri).
b. Anemia.
c. Leukemic retinopathy with papilledema.
d. Both b and c.
5. How should this patient be managed?
a. Immediate referral to the emergency room.
b. Referral to a neuro-ophthalmologist.
c. Panretinal photocoagulation.
d. Intravitreal Kenalog (triamcinolone acetonide) injection.
For answers, click here.
Discussion
A key piece of information not revealed in the medical history is that our patient had been diagnosed with acute myelogenous leukemia (AML) a year earlier. He underwent chemotherapy, and was thought to be in remission.
However, the bilateral disc swelling and other fundus changes seen probably represent a recurrence of the AML.
Leukemia represents a group of several cancers that affect the blood cells. There are four main types of leukemia: acute myelogenous, acute lymphocytic, chronic myelogenous and chronic lymphocytic.
AML is a malignancy that affects the white blood cells, either the granulocytes or the monocytes. It is the most common form of leukemia in adults, with an estimated 10,100 new cases per year.1
AML results in leukemic blasts; that is, an uncontrolled, exaggerated growth and accumulation of the white blood cells. AML also leads to a blockage in the production of normal marrow cells. This, in turn, can lead to a deficiency in the red cells, platelets and normal white cells, with resulting anemia, thrombocytopenia and neutropenia.
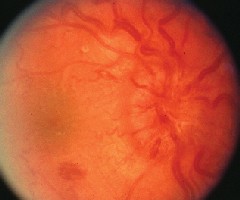
3, 4. The peripheral retina of each eye (O.D. right, O.S. left) showed suspicious retinal hemorrhages. There is obvious disc swelling in both eyes.

Ocular manifestations occur in about 90% of leukemia patients.2 Virtually all intraocular structures are involved, with infiltration of the optic nerve, choroid, retina, iris, ciliary body and anterior chamber. The most common retinal findings are dilation, tortuosity and beading of the retinal veins; retinal vascular sheathing; cotton-wool spots; superficial flame-shaped retinal hemorrhages; deep retinal hemorrhages; and white-centered retinal hemorrhages. These retinal findings may be the result of direct invasion of tissue by neoplastic cells.
Diagnosis is difficult, however, because many of these same retinal changes may occur in patients with severe anemia or thrombocytopenia. Also, leukemia patients often have severe anemia and thrombocytopenia, so it is difficult to know which of the three conditions is responsible for the retinal changes.
Retinal and choroidal infiltrates are more specific to leukemia. Retinal or preretinal infiltrates appear as gray-white nodules along the arcades and posterior pole.
Choroidal involvement is probably the most common site for ocular involvement of leukemia. The infiltration may not be visible on ophthalmoscopy, but it typically results in serous detachments of the retina or the pigment epithelium. This can often look like central serous chorioretinopathy or Haradas disease.
We were very surprised not only to see what appeared to be leukemic involvement in our patient, but also the extent of the involvement. There is obvious disc swelling in both eyes, probably due to leukemic infiltration of the optic nerves. This may also represent true papilledema from raised intracranial pressure, perhaps from central nervous system involvement of the leukemia.
Another striking finding: the white-centered retinal hemorrhages and dilated, tortuous retinal veins. These white-centered hemorrhages probably represent Roth spots.
Roth spots, initially described in patients with bacterial endocarditis, are known to occur with leukemia and severe anemia. In patients with bacterial endocarditis, the white area within the hemorrhage may contain the organism from a distant infection. In patients with anemia, the white area is more likely to consist of fibrin-platelet aggregates. The hemorrhages in patients with leukemia may be from direct infiltration of the leukemia cells.
This patient needs a medical work-up to see if the ocular changes represent a recurrence of his AML. The changes may also be due to severe anemia, or even a manifestation of blood hyperviscosity. A medical work-up would likely include a CBC with differential and bone marrow biopsy.
We referred our patient to the emergency room for evaluation and work-up. The patient did not return for follow up.
1. The Leukemia and Lymphoma Society, www.leukemia.org.
2. Dhaliwal RS, Schachat AP. Leukemias and Lymphomas. In: Ryan SJ, Schachat AP, Murphy RP, eds. Retina, Vol. IMedical Retina. 3rd ed. St. Louis: Mosby, 2000:842-57.

