Building a niche practice—any niche—is a challenging process that can yield emotional and financial rewards. A specialty contact lens practice comes with its own unique challenges, including managing the medical condition of a patient, navigating complex insurance coverage and designing and dispensing a custom product. My team and I have learned a lot from our experiences building our contact lens practice, and each year we find ourselves a little further ahead.
To have a successful specialty setting that optimally cares for patients, employees and doctors, you have to balance both clinical expertise and practice management know-how. While no one can argue the clinical skills need to be in place from the beginning, it is equally as important to ensure proper office protocols are in place. Staff education, insurance billing protocols, handling of custom contact lenses, schedule management and contact lens fitting documents or contracts are just a few aspects that are crucial in the management flow of a specialty contact lens practice.
When I asked myself, “If I were to start the practice all over again, what do I absolutely have to have in place to succeed?” I also considered parts of my practice that I wish were more efficient. While not a comprehensive list, here are some recommendations I have compiled from my experience to help you get your dream contact lens practice up and running.
Make Connections
A beautiful thing about specialty contact lenses is the community is so small. There are many resources available at your fingertips for both fitting and practice management techniques. To get started, reach out to those who have been there before. Relationships within the contact lens industry are particularly valuable and mutually beneficial. Attend events sponsored by the contact lens sections of major meetings, such as the American Academy of Optometry or American Optometric Association. A growing number of contact lens-specific meetings, such as the Global Specialty Lens Symposium and Vision by Design, are great places to connect with other like-minded practitioners for advice and guidance, not to mention the clinical training through CE courses. You are sure to meet an established contact lens fitter who is willing to share a few war stories and offer advice.
Additionally, connect with at least three specialty lens labs and get to know their consultants. Spend some time on the phone or at their exhibit hall booth and establish a relationship. Choose a lab that can do several types of gas permeable lenses, such as corneal spheres, bitorics and multifocals. Another lab can assist in your scleral lens contact lens fittings. Finally, establish an account with a custom soft lens laboratory.
Other lens options you might want to consider are orthokeratology and prosthetic contact lenses. Many labs can manufacture all types of lenses, but you will learn more working with consultants from a variety of backgrounds rather than a single group.
 |
| A multifunctional instrument that can assess topography, meibography and tear layer components provides a wide range of uses while maintaining a small footprint in the office. |
With this laboratory base, you will be able to order the right lenses for a large percentage of your patients. Great resources for researching lab options are the Gas Permeable Lens Institute (www.gpli.info) and the Scleral Lens Education Society (www.sclerallens.org).
Train Staff
Starting a specialty brings a new dimension to your office, and you’ll want to make sure your staff is prepared and on board with the changes in office protocols and patient communication. Take the time to educate your team about the types of lenses you’ll be fitting, the patient groups that might enter the practice and the ocular conditions that could benefit from specialty contact lenses. Also, review the basics of the types of contact lens solutions, eye drops, salines and application and removal tools you may be recommending. It’s helpful for some of your staff to be familiar with application and removal techniques of soft, corneal GP, hybrid and scleral contact lenses. Spending this time up front will save you, as the prescriber, many hours of phone calls and emails answering questions about contact lens solutions, wear times and whether or not a patient needs to return to the office for a follow-up appointment.
Simple Adjustment, Huge ImpactInvesting in technology can go a long way to building trust and loyalty with your patients. For example, a 38-year-old male with keratoconus presented to our clinic already wearing scleral contact lenses successfully. His only complaint was redness on his nasal conjunctiva during lens wear. Upon examination, we found his scleral lenses were compressing on a nasal pinguecula in each eye. With a simple depth and diameter measurement with an anterior segment OCT, we were able to order a microvault in a new pair of scleral lenses with near perfect dimensions, which relieved his complaints of redness. While I could have estimated the dimensions, the photos were great tools to not only efficiently prescribe his new scleral lenses, but also educate him on exactly what was occurring and how we fixed it. He has told his friends and family about his great experience, and that “we’re the office for great contact lenses.” As you know, word-of-mouth referrals are priceless. |
Update Office Protocols
Starting a specialty contact lens clinic within your practice is an investment with great potential. Understanding a few key aspects of running a practice using custom lens technologies will help protect those investments and allow the office to prosper. Here are four protocols to enact that will ensure a smooth specialty lens fitting process:
1. Patient information. The first protocol that should be in place is a fitting services brochure or contract, outlining both the office and patient responsibilities during the fitting process. This should be introduced and referred to during the initial visit. It is important for the patient to know the potential out-of-pocket costs and number of visits required to complete the lens evaluation. I have learned that patients are willing to pay out of pocket for high performing lenses and return for multiple visits when given proper notice. They do not appreciate, however, having to pay an unexpected amount or sitting through multiple evaluations when they had different expectations initially. The fitting brochure should include the price of services, if the office will bill medical or vision plans, when payments are due and if follow-up examinations are considered part of a global fitting period or as office visits billed to insurance. If there is a global fitting period, or a contact lens warranty period for remakes, the timing should be included in the fitting contract. Consider including examples of acceptable solutions and artificial tears that are compatible with their contact lenses, useful website links for application and removal tips, as well as any emergency contact numbers in case of needed care after hours.
2. Fitting information. To ensure you have the necessary information on the initial evaluation, develop a fitting protocol with the same basic information for every potential custom contact lens patient, regardless of condition. For example, a basic evaluation for someone with keratoconus could include history, visual acuities, refraction, slit lamp and topography. Adding technology such as endothelial cell counts, pachymetry and abberometry are helpful pieces of information.
A clinical pearl I have learned is to always take a baseline refraction for best-corrected spectacle acuities, even if vision is very poor, and be sure to document the best-corrected acuity obtained with a diagnostic contact lens plus the overrefraction results. Occasionally, insurances will request proof of significant vision improvement with a custom contact lens for lenses to be covered. Remind patients that you understand their vision is poor, but the measurements are for insurance purposes and baseline measures.
Educate and PreserveWhen working with specialty contact lenses, we often share good news with patients by showing them they can still see well despite their history of keratoconus, corneal scarring or other condition. However, we occasionally have to share less than favorable findings and educate patients about the maintenance therapy necessary to protect their eyes long term. For example, a 28-year-old female contact lens wearer mentioned moderate dry eye complaints and decreased contact lens wearing time. We noted significant meibomian gland dysfunction and lid margin telangiectasia. We educated her in office—using meibography photos from our multifunction topographer—about the damage that has already occurred to her meibomian glands, and that diligent maintenance is needed to protect the remaining glands. By comparing her photos to those of normal gland structure, she realized the importance of her care regimen and has committed to a follow-up schedule and filling her prescriptions. |
After baseline testing, make sure patients don’t have other questions about the fitting period, any available warranties and exchanges for lenses, and how any potential out-of-pocket costs are handled. Once the patient agrees to the fitting protocol, you can begin the contact lens fitting with diagnostic lenses; the visit could be considered complete if you decide to order empirically. Some practitioners prefer the patient come back for a second fitting visit, while others perform the fitting on the same day. In our office, we gauge a patient’s interest in a screening visit only vs. a lens fitting and book time accordingly.
3. Organization. Another key office protocol in managing your contact lens clinic is how to organize and manage lenses delivered to the office. The first step in this process is understanding your laboratory’s warranty process. Each lab has a number of lens orders and a certain number of days adjustment lenses can be ordered for little-to-no cost after purchasing the first set of lenses. Some labs require return of each lens set to send adjustment lenses, while others require return of lenses only if the entire order is cancelled within the warranty period. Therefore, it’s imperative you keep all lenses accounted for to return lenses needed for credit. Without a proper lens management system in place, fitting specialty contact lenses can get very expensive. A posted chart referencing each lab’s exchange policies can be helpful in deciding how lenses should be organized.
Some examples of lens management systems could include a tray or file system, where flat-packs or small bags are kept and labeled with the lens order date, reference number or some other identifying method. I find it helpful to keep the lens invoice with the previous lenses for quick reference of previous and current lens parameters. Once the fitting is complete, we scan all invoices to the patient record. This makes it easy to keep track of which lenses the patient most prefers; it also simplifies returns to the laboratory, if needed. We also keep a flow sheet with the lens tray for quick notes to others in the office. At the end of each visit, anything the rest of the office should know for the patient’s next visit can be noted, such as needing to return previous lenses for credit, if the lens fitting is finalized or if the patient has a balance after insurance processing.
As offices move toward paperless records, managing this type of inventory can get tricky, and it is vital to have a solid system in place. A single missing lens, or not returning lenses under warranty in a timely manner can cost the office hundreds of dollars each month. It is not unreasonable to dedicate a staff member to this project as your patient base wearing specialty contact lenses grows.
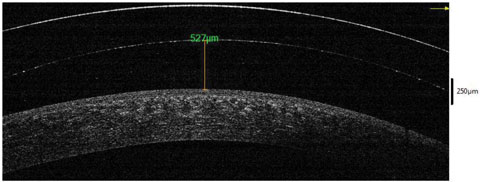 |
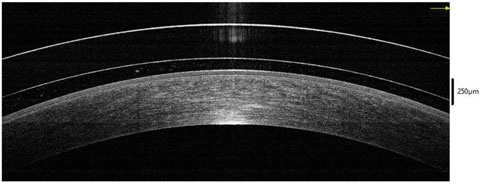 |
| OCT images such as these can assist in scleral lens assessment at the corneal apex and limbal areas. The top image depicts extra vault, while the bottom image shows proper vault. |
4. Backup plan. Lastly, be sure to create an office policy on how cases are handled when the patient decides they do not want to go forward with the lens fitting. This policy should address if there is any potential for refunds on returned lenses and how service fees are handled if the fitting is not yet complete. Thankfully, this happens far less than patients completing their fitting, but when you do have this situation, it’s much easier to handle with a protocol in place beforehand, the entire staff is aware of the policy and everyone knows how to explain it to the patient. A brief explanation of this policy should be in the contact lens fitting brochure or contract.
Build Clinical Skills
Managing the clinical side of the practice is the easy part of a specialty contact lens practice. With the available webinars, hands-on workshops and consultation teams, information is always readily available to assist you in fitting custom contact lenses.
The first step in learning the skills needed to fit custom contact lenses is identifying the right candidates. In general, most myopic children are great candidates for orthokeratology, and many patients with irregular corneas will appreciate the vision and comfort of scleral contact lenses. However, there are groups of patients that are not ideal candidates for certain lens designs. Patients with a low endothelial cell count after a corneal transplant surgery are not ideal candidates for scleral contact lenses due to potential for corneal edema. Numerous resources, including the websites mentioned previously, consultants, research databases and lectures at state and national meetings will often review the ideal candidates for each particular lens design.
With any lens design, consider starting with and learning from a patient who is considered mild in the condition you are treating. For example, begin your orthokeratology fitting with a -2.00 myope rather than a -7.00, as the need for complex troubleshooting techniques will be lower with such a patient. If you would like to start fitting scleral lenses, consider starting with a patient who has mild keratoconus. These types of patients will help you learn and gain confidence at the same time. It is also helpful to discuss your fit with the consultation team, to make sure you are completing the necessary clinical assessments. As you complete more fittings and master the common patient symptoms and how an appropriately fit lens performs, you can broaden your patient base to those with more severe forms of their conditions.
Specialty contact lenses are still contacts, and the fitting assessments should have the same flow as evaluation of a non-custom lens. Measure vision, complete an overrefraction and fitting assessment and evaluate the cornea with sodium fluorescein after removing the lenses. The key is being aware of the evaluation points of the fit and recognizing when findings indicate a refit or routine monitoring of corneal health.
Invest in Technology
Some additional tools can make you more efficient at fitting custom lenses and can assist in troubleshooting difficult fits. These procedures are also billable to medical insurances when a medical diagnosis and applicable plan is involved. Consider investing in these instruments to build your practice and knowledge of how specialty contact lenses affect the ocular surface:
• Corneal topographer: This tool is a must if you plan to fully manage corneal diseases and dystrophies. For keratoconus in particular, being able to manage not only the contact lens fitting but also monitor for progression is key. A topographer is also especially helpful in troubleshooting and monitoring orthokeratology fittings. Topographers that can scan the posterior cornea, also known as the posterior float, can be particularly beneficial in explaining why a patient with an irregular cornea and little-to-no corneal scarring has limited visual acuities. New technologies in some topographers allow us to scan the scleral shape to maximize the shape design of the landing zone curves of a scleral lens.
• Anterior segment OCT: This is a fantastic tool to assess scleral contact lenses beyond what we can see with the slit lamp. Quantifying corneal and limbal vault is remarkably helpful in troubleshooting, as is monitoring for corneal edema over time. I find this instrument particularly helpful in managing patients with corneal transplants to minimize the lens vault, which maximizes oxygen transmission while ensuring complete lens clearance over the graft-host junction.
• Specular endothelial microscopy: Specular microscopy is another great baseline and troubleshooting measure when working with patients wearing specialty contact lenses. Particularly helpful on patients wanting to wear scleral lenses, these measurements can help you decide if the cornea can handle a scleral lens system without becoming edematous.
Educating Others About Your Practice
There are a few final pieces to add to your specialty practice, especially if you plan to work with other local medical professionals. Stock up on basic brochures about conditions and procedures such as keratoconus, corneal transplants, orthokeratology and scleral lens fittings to quickly answer patient questions and provide a resource they can take with them. A professional brochure about your practice is a perfect way to build referrals from other local optometrists, ophthalmologists and other medical professionals.
As your relationship with local professionals grows, prepare a template to send back to referring providers with information about your findings and the plan for your mutual patient. Respectful comanagement will go a long way in your continued practice growth. Much like our ophthalmology colleagues after cataract surgery, be sure to recommend patients back to their referring provider for services such as back-up glasses and red eye evaluations, especially in instances not related to their contact lens wear.
The Sky’s the Limit
As contact lens technology continues to grow, so will our ability to fit lenses with more precision and efficiency. We are already getting a taste of measurements that can customize lens optics to maximize vision, add prism and control aberrations. One day specialty contact lenses may become mainstream in monitoring medical conditions such as diabetes and glaucoma. Thankfully, our offices are ready to handle these innovations now.
Dr. Messer received her doctor of optometry degree from Southern California College of Optometry, and completed a cornea and contact lens residency. She now practices in Edina, MN, with special interests in scleral, multifocal and orthokeratology contact lenses.
Dr. Messer is a consultant for CooperVision and Precilens, has research funding from Bausch + Lomb and is a Residency Forum Coordinator for Alden Optical.

