
As primary-care optometrists, we see myriad ocular conditions ranging from convergence insufficiency to angle- closure glaucoma. Our job is to effectively diagnose and manage each situation to ensure the best outcome for our patients.
But, what happens when the patient has undergone enucleation and is now anophthalmic? How do you provide eye care when an eye no longer exists? In this months column, well review some common problems that anophthalmic patients experience and how to manage them.
The Anophthalmic Socket
Anophthalmic patients present a unique challenge. Although there is no eye, these patients are susceptible to adnexal infections, allergy and inflammation. Also, the anophthalmic patient is predisposed to eyelid positioning abnormalities, so a poorly fit prosthesis can cause discomfort and compromise cosmesis. Proper evaluation and management is required to appropriately address these patients needs.
This starts with a thorough history. Ask about the age of the prosthesis, how frequently it is removed and cleaned, and if the patient visits his or her ocularist regularly.
Also, note if the involved eye appears proptotic or enophthalmic with the prosthesis in place and if there is good translation of the prosthesis as the patient looks from side to side. Prostheses that are too small and poorly fit often do not move well and can become displaced; a secondary ptosis is also possible. Likewise, prostheses that are too large can cause pain and incomplete lid closure.
We recommend removing the prosthesis and examining the anophthalmic socket. If you are uncomfortable with or inexperienced at doing this, ask the patient to remove it. Most prostheses can be removed by simply retracting the lids and applying pressure to the edge, although some have elaborate designs that consist of pegs and/or magnets.
Once the prosthesis is removed, inspect the underlying tissue. The conjunctiva should be pink and free of papillae or follicles. Excessive redness and edema may indicate inflammation. Look carefully for purulent or ropy mucous discharge that emanates from the walls of the anophthalmic socket and collects either on the surface of the conjunctiva or in the inferior cul-de-sac; this suggests conjunctival compromise. Be aware of any foul odor emanating from the socket, as this may signify infection.
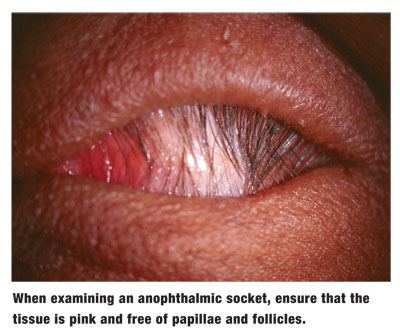
Ensure that the socket is fully closed, and that the orbital implantusually composed of high-density porous polyethylene or coralline hydroxyapatite1has not extruded through from the orbit. This is crucial; any compromise of the socket provides a direct route for potential spread of infection to the orbit and, ultimately, the intracranial cavity.
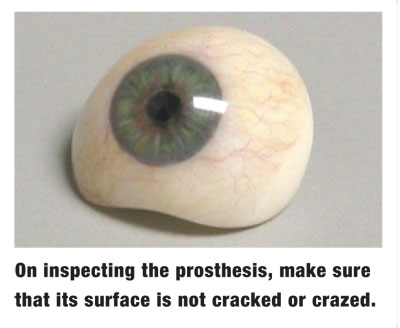
Also, inspect the prosthesis itself. Ensure that the surface is smooth and not crazed or cracked, as these imperfections can harbor microbial pathogens.
The Maladies
Bacterial infection in the anophthalmic patient is typically acute. Such patients present with an accumulation of mucopurulent discharge, localized pain and swelling of the ipsilateral lids and periocular tissue. For management, we typically prescribe a broad-spectrum antibiotic such as Vigamox (moxifloxacin 0.5%, Alcon) because of its convenient t.i.d. dosing schedule. If the inflammation is significant, consider prescribing a concurrent topical corticosteroid q.i.d. to q2h, depending on the severity. The drops are instilled directly into the anophthalmic socket, not over the prosthesis.
Giant papillary conjunctivitis (GPC) is another common malady in anophthalmic patients. Symptoms include discomfort and displacement while wearing the prosthesis and a ropy mucous discharge. Biomicroscopy reveals large papillae on the tarsal plate and bulbar conjunctiva.
Although we often use mast cell stabilizers to manage GPC in contact lens patients, we tend to rely heavily on corticosteroids for individuals with prosthesis-induced GPC. The primary risks associated with topical steroidselevation of intraocular pressure and cataractogenesisare irrelevant in the case of the anophthalmic patient.
Anophthalmic patients may exhibit diminished orbital volume over time due to atrophy of orbital fat. Also, acquired eyelid laxity and dehiscence of the levator muscle can lead to ptosis or involution of the lids, manifesting as entropion.
Improperly fitted prostheses can also cause these problems. Ensure that the prosthetic eye is of the correct size and thickness for the anophthalmic socket. If not, refer the patient to an ocularist for modification or replacement.
If the prosthesis is adequate, the patient may require surgical augmentation of the orbit. Problems with ptosis may be addressed by building up the prosthesis superiorly to better support the upper lid or by performing a surgical resection of the levator muscle.2 Entropion is typically addressed surgically as well, either with a lid resection or a suture placement in the lid sulcus to rotate the eyelids outward.3
Implications of Monocular Vision
The loss of one functioning eye diminishes a patients field of vision by 15% to 20%.4 Additionally, these individuals suffer a complete loss of stereopsis, which can compromise their hand-eye coordination and ability to accurately judge distances. Decreased overall acuity is also likely, since monocular patients do not benefit from binocular summation. There is also the potential for impairment in spatial orientation, which results from a lack of kinesthetic cues that arise from convergence and accommodation.5
Patients are most susceptible to these issues in the early weeks and months following enucleation.6 Those who are born monocular or who have been monocular for a long time tend to adapt relatively well. Most monocular patients unconsciously alter their head posture and increase head movement to compensate for loss of visual field and ocular motility.
Special attention and care are required for activities such as navigating stairs or curbs, crossing busy streets and, especially, driving. Monocular drivers have, on average, seven times more accidents than the general population.7
While no treatment can fully restore the peripheral field or binocularity, low vision rehabilitation can often improve visual function, allowing anophthalmic patients to better function in their environments and perform daily activities. The use of mirrored systems and visual scanning techniques are just some of the available options for these individuals.5
Monocular patients must be educated about the need to safeguard their remaining functional eye. Protective eyewear with polycarbonate lenses is vital.
While the anophthalmic patient faces many challenges, an educated and compassionate optometrist can help to ease this burden and ensure the continued health of the remaining tissue. As 15th-century philosopher Erasmus wrote, In the kingdom of the blind, the one-eyed man is king. In other words, even partial vision is precious.
1. Su GW, Yen MT. Current trends in managing the anophthalmic socket after primary enucleation and evisceration. Ophthal Plast Reconstr Surg 2004 Jul;20(4):274-80.
2. Murchison AP, Bernardino CR. Evaluation of the anophthalmic socket. Rev Ophth 2006 Sept; 13(9):76-80 .
3. Barnes JA, Bunce C, Olver JM. Simple effective surgery for involutional entropion suitable for the general ophthalmologist. Ophthalmology 2006 Jan; 113(1):92-6.
4. Keeney AH. Current transitions in ophthalmic aspects of licensure for motor vehicle drivers: problems, hazards, and working solutions. Trans Am Ophthalmol Soc 1993; 91:197-202; discussion 202-6.
5. Politzer T. Implications of acquired monocular vision [online]. NORA: Neuro-Optometric Rehabilitation Association. 2004. Available: www.nora.cc/patient_area/monocular_vision.html. (Accessed February 12, 2007.)
6. Linberg JV, Tillman WT, Allara RD. Recovery after loss of an eye. Ophthal Plast Reconstr Surg 1988; 4(3):135-8.
7. Keeney AH, Singh GC, Berberich S, Giesel J. Evaluation of the driver limitation program in Kentucky 1964-1984. J Ky Med Assoc 1985 Jun;83(6):327-31.

