 |
Q:
A 23-year-old African-American female presented for a routine annual eye exam. Dilated retinal exam and imaging revealed a well-circumscribed macular lesion OD, with areas of hypo- and hyperpigmentation. What is in the differential diagnosis for this patient, and what needs to be done?
A:
“Pigmented macular lesions in young patients are always worrisome and deserve careful attention to arrive at the correct diagnosis,” says Alexander Bottini, MD, retina specialist at Omni Eye Services in Atlanta. “Structure your list around either an infection, a neovascular process, a neoplasm or a congenital lesion.”
In young patients with pigmented macular lesions, consider TORCH syndrome—congenital infection of Toxoplasmosis, Other agents (e.g., syphilis, parvovirus),Rubella, Cytomegalovirus or Herpes simplex virus.
Congenital toxoplasmosis, in particular, can leave behind large and devastating chorioretinal scars in the macula.
List of Lesions
 |
|
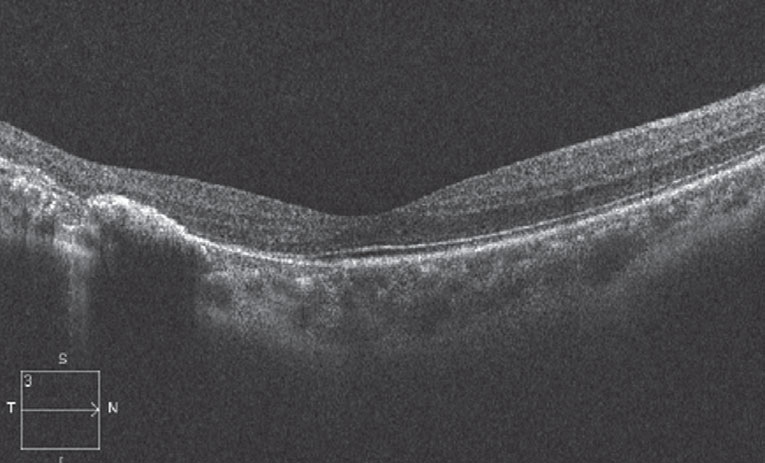
Outer retinal changes on the OCT (above) are apparent in the location of the torpedo lesion (below). Click image to enlarge. |
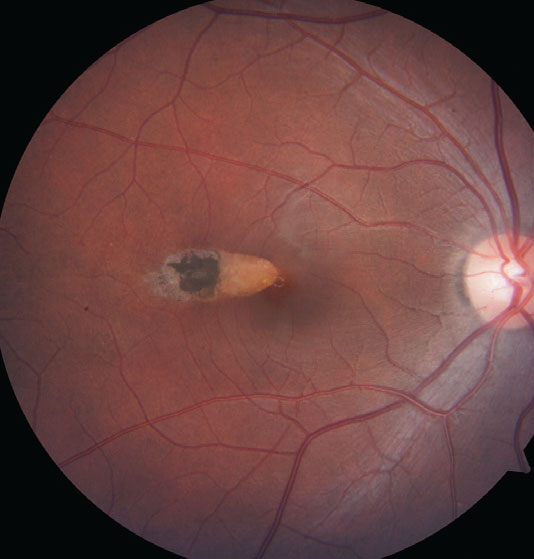 |
| Click image to enlarge. |
Any choroidal neovascular membrane (CNVM) in a young patient needs a good explanation. High myopia could be the culprit, so it’s essential to know the patient’s refraction. Remote ocular trauma with an asymptomatic choroidal rupture can result in CNVM years later. A young patient with CNVM who grew up near the Mississippi or Ohio River valleys is always a suspect for presumed ocular histoplasmosis syndrome. White dot syndromes, particularly punctate inner choroiditis and multifocal choroiditis and panuveitis, should also be on the differential.
Choroidal lesions—nevi, melanomas and metastases—can occur in the macula. On exam, these lesions are deep to the retina. To distinguish melanomas from nevi, look for subretinal fluid, orange pigment and significant elevation of the lesion.Congenital hypertrophy of the retinal pigment epithelium (CHRPE) lesions are often seen in the periphery, but the well-circumscribed, pigmented lesions of the outer retina can occur in the macula. Congenital simple hamartoma of the RPE lesions are more rare but can also appear in the retina as focal, densely pigmented lesions that often extend into the inner layers.
Ocular Torpedo
This patient’s fundus appearance happened to be a classic presentation of torpedo maculopathy—an oval-shaped lesion in the temporal macula with a hypopigmented, tapered tip pointing toward the fovea and a sometimes hyperpigmented tail extending temporally.1 RPE attenuation and photoreceptor layers are seen on OCT. Patients are almost uniformly asymptomatic.
“Regarding pathogenesis, we simply don’t have a definite answer,” Dr. Bottini says. “We know it to be a congenital lesion, so various insults occurring during retinal development—such as an intrauterine infection or vascular abnormality—have been suggested.” There is a strong suspicion that the lesion arises during the specific period in fetal development where we see the so-called “fetal temporal bulge”—a dense but transient clustering of RPE cells in the temporal macula.2 Both the size and shape of the fetal temporal bulge correlates with the torpedo lesions.2,3
“While torpedo maculopathy lesions are often incidental findings that pose no threat to the eye, they can rarely develop a CNVM, so monitor them as needed. Dr. Bottini says. “Areas of dense hyperpigmentation within the lesion, such as those seen in this case, should raise one’s suspicion and prompt multimodal imaging to look for a CNVM.”
Even if a CNVM is not present, these patients should be educated in the use of an Amsler grid and followed about every six to 12 months.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
1.Roseman RL, Gass JD. Hypopigmented nevus of the retinal pigment epithelium in the macula. Arch Ophthalmol. 1992;110(10):1358-9. 2. Shields CL, Guzman JM, Shaprio MJ, et al. Torpedo maculopathy at the site of the fetal “bulge”. Arch Ophthalmol. 2010;128(4):499-501. 3. Shirley K, O’Neill M, Gamble R, et al. Torpedo maculopathy: disease spectrum and associated choroidal neovascularisation in a pediatric population. Eye (Lond). 2018;32:1315-20. |

