Q: I recently attended a lecture on viral eye disease in which the speaker differentiated between mucous plaques and dendriform lesions in herpes zoster that might harbor live virus. Do they respond to topical antivirals? How can I make the distinction between those lesions that are possibly treatable with antivirals vs. those that would likely not respond to antiviral treatment?
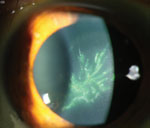 | |
| Pseudodendrites present as an acute keratitis within a month after skin lesions. Image: Christine W. Sindt, OD. | |
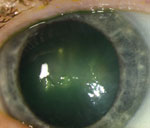 | |
| A mucous plaque stained with rose bengal dye. Image: Christine W. Sindt, OD. |
A: “It is often difficult to distinguish on clinical exam (i.e., slit lamp examination) between true herpes zoster mucous plaques, which are virtually always noninfectious, [and] various herpes zoster dendriform lesions, which, depending on the timing of the culture, may or may not harbor live virus,” says Vincent de Luise, MD, assistant clinical professor or ophthalmology at Yale University School of Medicine. “Both types of lesions can appear as elevated, plaque-like, medusoid epithelial lesions with variable staining patterns to rose bengal, lissamine green and fluorescein, although mucous plaques usually are much larger and pleomorphic.”
Dr. de Luise says that the FDA has not yet approved any topical antivirals for use against the herpes zoster virus (VZV) when it manifests as keratitis. “Off-label topical trifluridine 1% solution is rarely effective,” he notes, while “the off-label use of topical ganciclovir 0.15% gel may have some efficacy. Oral antivirals have not demonstrated efficacy in any consistent manner.” He adds that short courses of topical corticosteroids, with careful follow-up, can be used to treat herpes zoster nummular keratitis and herpes zoster disciform keratitis, as well as other manifestations that are inflammatory in nature. But, that is not the case with herpes zoster mucous plaques or infectious zoster dendriform keratitis.
Jason Duncan, OD, associate professor at the Southern College of Optometry, recommends use of ganciclovir gel should you decide you are dealing with dendrites associated with zoster ophthalmicus. Ganciclovir gel may be less toxic to the cornea when compared to other topical antivirals that are successful in treating dendritic keratitis associated with simplex disease. This becomes important to consider because the length of topical antiviral treatment may be longer and the taper more extended when dealing with zoster ophthalmicus. Also, “you must be sure that you are dealing with epithelial lesions, as zoster ophthalmicus often produces corneal stromal lesions, or nummular keratitis. The appropriate treatment for such lesions is the judicious use of topical steroids in conjunction with some form of antiviral therapy,” Dr. Duncan says. Gancyclovir gel is typically prescribed five times daily until the epithelial lesion has healed and then used for an additional two to four weeks BID.
Mark Abelson, MD, founder of Andover Eye Associates in Massachusetts, points out that regardless of the type of lesion, the virus strain should respond similarly to antivirals unless the patient harbors an antiviral resistant strain. “The distinction should be based upon empirical assessment with an appropriate course of antiviral therapy,” he says, adding that patients should be informed that the treatment provides symptomatic relief, but that the virus will remain in a latent state even when no symptoms are obvious. He recommends encouraging all patients over 50 years of age to receive immunization against herpes zoster to prevent possible recurrences.
