 |
Q:
An 18-year-old female presented for a routine exam with no visual complaints, but confrontation visual fields revealed an inferior defect in one eye. What tests should I perform and what is in the differential diagnosis?
A:
"Many causes of a visual field defect are easily recognized, such as a retinal detachment or glaucoma,” says Paul C. Mitchell, OD, of Eye Care of Delaware. “Others are more elusive and require an extensive work-up.” He adds that uncovering the etiology of less common conditions always requires a more deliberate evaluation. Investigating retinal, optic nerve and optic pathway causes is essential.
Start with in-office testing, including a thorough history, best-corrected vision, pupils, color vision, intraocular pressure, dilated eye exam, formal visual fields and OCT. B-scan ultrasound, fluorescein angiography and fundus autofluorescence (FAF) may also be necessary.
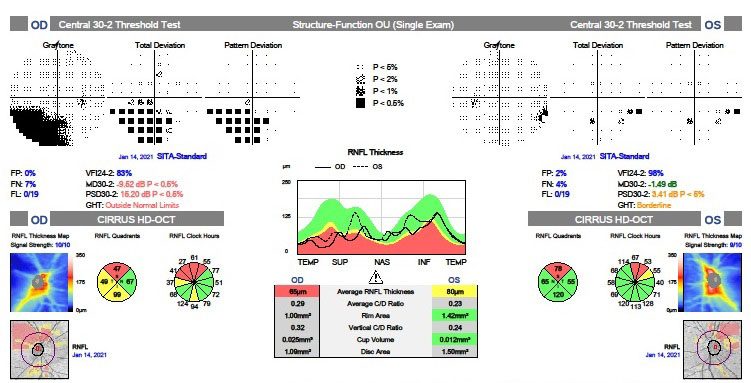 |
Figs. 1 (top) and 2 (bottom). VF and OCT as well as fundus images are useful in diagnosing SSOH. Click images to enlarge. |
 |
Element of Surprise
The patient’s visual acuity was 20/20 OU. Pupillary testing showed no afferent defect. Confrontation fields showed a defect inferiorly OD. Pressures measured 16mm Hg OU. Visual fields disclosed inferior altitudinal defects greater in the right eye than left (Figure 1). OCT revealed superior RNFL loss OU with a single peak. Superior ganglion cell layer loss was also noted. Careful optic disc exam showed a superior entrance of the central retinal artery and vein with loss of optic nerve tissue adjacent to it. There was no disc edema or pallor (Figure 2). B-scan ultrasound and FAF ruled out optic nerve head drusen. An MRI was ordered and was negative. Based on the appearance of the optic nerve, OCT and visual field defects, a diagnosis of bilateral superior segmental optic nerve hypoplasia (SSOH) was made.
SSOH, or “topless disc syndrome,” is a form of optic nerve hypoplasia. There is loss of nerve tissue superiorly on the disc with a relative superior entrance of the central retinal artery and vein. There can be superior pallor and a superior peripapillary halo adjacent to the disc. OCT findings typically show loss of the RNFL superiorly with a single peak and a corresponding inferior visual field defect. This condition tends to be nonprogressive.
“Because this is a congenital condition, most patients are unaware of their visual field loss, and central vision remains good,” Dr. Mitchell says. He notes females are more affected than males, there is an association with gestational diabetes and the condition occurs in 0.3% of Asians.1-4
Check for Signs
When evaluating a young patient with field loss, look at the disc for signs of drusen, optic pit or glaucoma. Consider a B-scan or FAF to detect buried drusen. A B-scan would show a highly reflective nodule and FAF would exhibit autofluorescence. A history of sudden vision loss and pain with eye movement would point toward an inflammatory event such as optic neuritis. Check color vision, pupils and order an MRI of the brain and orbits to confirm the diagnosis of optic neuritis. Look at the visual field pattern along with disc pallor or swelling that might indicate an intracranial cause. Careful dilated retinal exam is also key.
“During every eye exam you perform, routine or not, confrontation fields are critical and may be the only clue of an ocular disorder,” Dr. Mitchell notes. In our patient, a careful disc exam with ancillary testing confirmed SSOH. We expect her nerves and visual fields to be stable over time.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
1. Seo S, Lee CE, Kim DW, et al. Prevalence and risk factors of superior segmental optic hypoplasia in a Korean population: the Korea National Health and Nutrition Examination Survey. BMC Ophthalmol. 2014;14:157. 2. Purvin VA. Superior segmental optic nerve hypoplasia. J Neuro Ophthalmol. 2002;22(2):116-7. 3. Kim RY, Hoyt WF, Lessell S, Narahara MH. Superior segmental optic hypoplasia: a sign of maternal diabetes. Arch Ophthalmol. 1989;107(9):1312-5. 4. Yamamoto T. Superior segmental optic hypoplasia as a differential diagnosis in glaucoma. Taiwan J Ophthalmol. 2019;9(2):63-6. |

