
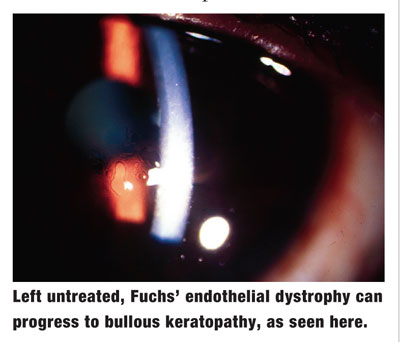
Q: I have a patient who has Fuchs endothelial dystrophy and a significant cataract. Im hesitant to recommend cataract surgery due to possible corneal decompensation. What should I do?
A: Penetrating keratoplasty (PK) has been the standard of care for patients who have Fuchs endothelial dystrophy. But, cataract surgeons may tend to put off operating on such patients because visual recovery for PK patients can take up to a year or more, says optometrist Edward J. Wasloski, clinical director of Omni Eye Specialists, in
But, a new, less invasive procedure removes only the diseased endothelial layer and Descemets membrane, not the full-thickness cornea as in PK. This new procedure allows vision to recover within weeks instead of many months, Dr. Wasloski says. Plus, visual outcomes are exceptionally better, and there are no corneal sutures.
The procedure is commonly known as Descemets stripping endothelial keratoplasty (DSEK). Its also called Descemets stripping automated endothelial keratoplasty (DSAEK) because of the automated microkeratome used to cut the donor tissue, or Descemets stripping lamellar endothelial keratoplasty (DSLEK).
Fuchs patients in need of cataract surgery can now proceed with cataract removal. If the cornea decompensates, DSEK can be performed at the appropriate time, says Ivan H. Garcia, M.D., medical director at
In DSEK, the surgeon strips away about an 8mm circle of endothelium through a small surgical incision. Then, a thin (100m to 200m) disc of donor endothelial tissue is cut, coated with viscoelastic to protect it, folded like a taco, and slid through the incision into the anterior chamber.
Unfolding the tissue can be the tricky part, Dr. Garcia says. But once that is done, the donor tissue is positioned, and an air bubble is injected to hold it in place and help it bond to the host tissue. If the graft doesnt adhere firmly in the first postoperative week, another air bubble can be injected, usually in an in-office outpatient procedure.
Q: How does the post-op care for a DSEK patient compare with the post-op care of a PK patient?
A: The post-op care is very similar to that for PK, and these patients require a lot of handholding during the first few weeks after the procedure, when dislocation is most likely, Dr. Garcia says. Patients are prescribed an antibiotic, such as Vigamox (moxifloxacin, Alcon), to be used q.i.d. until the bottle is depleted (i.e., about a week to 10 days), and a topical steroid, such as Pred Forte (prednisolone acetate, Allergan).
Patients usually remain on the steroid indefinitely. As long as the intraocular pressure does not go up, I leave them on the Pred Forte, Dr. Garcia says. He tries to return patients to the comanaging optometrist by four to six weeks post-op. If patients are doing well, they may be ready for a temporary visual correction at that time.
Meanwhile, O.D.s should carefully monitor the patients healing. A warning sign to look for is unusual redness of the eye, which could indicate either early rejection (graft failure) or a mild late infection. Send this patient back to the surgeon immediately.
As in PK, graft rejection is still a possibility in DSEK. There are no data yet to say whether rejection is less common in DSEK, but Dr. Garcia and other surgeons think this is likely. I consider this procedure a major breakthrough, in all honesty, in the way corneal transplants are being done, he says.

