We are at the beginning of a revolution in the area of genomics and genetics. This revolution is changing our roles as primary care providers.
The old genetics dealt with the rare, single gene (monogenic) diseases like retinitis pigmentosa and Marfans syndrome, as well as chromosomal abnormalities such as Down syndrome. But the new genetics deals with the multifactorial diseases caused by genetic and environmental factors. These are the much more common diseaseslike glaucoma and macular degeneration, as well as heart disease and diabeteswhich you see in your office every day.
The Human Genome Project and other recent advances are exponentially increasing our knowledge of genetic conditions. Because of this rapid rate of increase in our knowledge, because of the paradigm shift from the old genetics to the new genetics, and because of the fact that the clinical applications of the genomics revolution are beginning to filter into our practice, we need to become familiar with the new concepts and principles of genetics and genomics. We need to be able to apply this new information in our practices and keep up with the advances that are relevant to our patients. To do this, begin with the following eight steps.
1. Expand your differential diagnoses to include genetic disorders.
Essentially all disorders (except possibly trauma) have a genetic component.1 In terms of the new genetics, the most common diseases you see in practice are the multifactorial disorders that involve multiple genes interacting with environmental influences. Examples of multifactorial systemic disorders are Type 1 and Type 2 diabetes, hypertension, heart disease, asthma, cancers and Alzheimers disease. Ocular disorders that are multifactorial include the glaucomas, age-related macular degeneration, cataracts, myopia and diabetic retinopathy.
Thus, when you are examining a patient, assume that all disorders have some genetic component. Learn to think genetically. You are not required to become an expert in genetics, but you should start to incorporate genetic thinking and genetic principles in your delivery of eye care. This can start with a genetic test you administer to all of your patients: the family history.
You already take a family history as part of your initial comprehensive examination of a patient.
Because of the genomics revolution, the purpose and scope of taking a family history have changed. The increasing role of genetics means that you need to expand your family history to include information on genetic factors. This will help you to identify genetic susceptibilities or conditions in your patients, make an early diagnosis, identify at-risk family members, establish the type of inheritance, determine risk level, and educate/reassure patients. In addition, the information you obtain in the family history is often the first way to identify patients who are candidates for genetic testing, for preventive measures, for monitoring or for referral.
| Symbol Legend: White Square/White Circle = Unaffected BlackSquare/Black Circle = Affected |
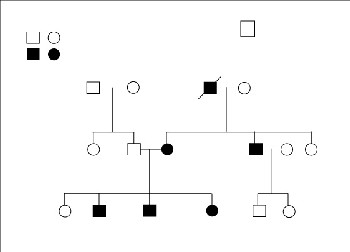 |
| Sample family pedigree of three generations. |
In select cases, the family history information should be converted into a diagram of the biological relationships of your patient with his or her family membersa pedigree. This is especially true in cases where an ocular disease appears to run in the family or where vision loss occurs at an earlier age than the typical onset. At a minimum, you should draw a three-generation pedigree, including your patients children, siblings, parents, aunts, uncles, nephews and nieces. If your patient is a child, then the pedigree would include the patients siblings, parents, aunts, uncles, nephews, nieces and grandparents.
The pedigree is a simple, effective tool to help you visualize how diseases or conditions are clustering within families and how they move through the different generations. This can then help you diagnose, assess risk, educate, and treat or refer. You should update the pedigree on subsequent visits.
Family history tools have been designed for use by the public and are available on the Internet. One tool was jointly designed by the American Society of Human Genetics, Genetic Alliance and the National Society of Genetic Counselors. (See table, Web-based Resources for Clinical Genetics, on page 64.) To minimize your chair time devoted to the taking of this information, the patient can access this tool online at the web sites of any of the three organizations, find and fill out the information, and bring it to your office.
| Genetics and Genomics Defined |
| Genetics: The study of the patterns of inheritance of specific traits. Genomics: The study of the function of genes and their full SDNA sequences (i.e. genomes). |
A good resource for information is the March of Dimes clinical genetics program that contains a module on family history
(www. marchofdimes.com/gyponline/index.bm2). This is an excellent web site that contains clinically useful information in three modules: genetic testing and screening, family health and social history, and referral to genetic services.
Another excellent resource is the book The Practical Guide to the Genetic Family History, by R.L. Bennett (John Wiley, 1999).2
3. Learn the genetics of the disorders you see most often in your practice.
You need to be aware of the genetic contributions to the common ophthalmic conditions you see in practice. There has been a tremendous advance in our knowledge of the genetics of these conditions. For example, there are excellent reviews available on the genetics of the glaucomas,3,4 age-related macular degeneration,5,6 cataracts,7,8 myopia,9,10 neuro-ophthalmic disorders,11 corneal dystrophie 12,13 and retinal dystrophies.14,15
As more and more is discovered about the genetics of these disorders, you will have more diagnostic tests available to you and eventually more treatment options. You will also have more information to help your patients understand their conditions, to help them make decisions, and to provide supportive counseling.
|
Web-Based Resources for Clinical Genetics |
| Resource | URL |
| American College of Medical Genetics | www.acmg.net |
| American Society of Human Genetics | http://genetics.faseb.org/genetics/ash/ashgmenu.htm |
| ClinicalTrials.gov | http://clinicaltrials.gov/ct/gui |
| Gene Tests | www.genetests.org |
| Genetic Alliance | http://geneticalliance.org |
| Genetics and Your Practice | www.marchofdimes.com/gyponline/index.bm2 |
| National Coalition for Health Professional Educationin Genetics | www.nchpeg.org |
| National Human Genome Research Institute | www.nhgri.nih.gov |
| National Organization of Rare Disorders | www.rarediseases.org |
| National Society of Genetic Counselors | www.nsgc.org |
| Online Mendelian Inheritance in Man (OMIM) | www.ncbi.nlm.nih.gov/omim |
| PubMed | www.ncbi.nlm.nih.gov/entrez |
| RetNet (Retinal Information Network) | www.sph.uth.tmc.edu/Retnet |
4. Learn how to appropriately order and interpret selected genetic tests.
The number and availability of genetic tests for ocular conditions will increase in the future. So will the pressure to use these tests. You should be familiar with the GeneTests web site in order to identify labs that offer specific genetic tests. (See table above.) The GeneTests site informs you of both commercial and university labs. Research labs do not offer clinical testing, but some of them accept direct contact from patients for possible inclusion in a research study. Check the GeneTests web site to see if the lab accepts direct contact from patients.
As an alternative, check the Clinical Trials.gov web site. This site gives you participation and contact information about federally and privately supported clinical research.
One genetic test that is commercially available is the OcuGene test for myocilin glaucoma.16 Mutations in the myocilin gene are responsible for many cases of juvenile-onset open-angle glaucoma and for 3-5% of primary open-angle glaucoma.17 Although this is not a good screening test for the general population, it may be useful in testing a patient, for example, who has a number of family members with early-onset open-angle glaucoma. In a family with members who have a myocilin mutation, other family members should be tested as early as possible. If a family member does not have that mutation, that persons risk of glaucoma changes from 50% to about 2% (i.e., the risk of the general population).18 But if the test is positive, treat the family member as a glaucoma suspect. If the glaucoma workup is negative, then increased surveillance is indicated.
There is still controversy associated with the significance of the MYOC.mt1 promoter region variant identified by this test, and there is a need for further studies. Even so, if you offer this test to a patient, you should be able to educate and counsel your patient to get truly informed consent and be able to interpret the results of the test to the patient. If you dont feel comfortable doing this, or if this is your first attempt to offer a test, consult a genetics professional who can help you with the process and the interpretation.
5. Learn how genes affect populations and how this influences individual risk.
The risk of a particular disease may be greatly increased in a specific population or ethnic group. This may warrant screening in patients of that population. Examples include congenital glaucoma in an Amish population, retinoschisis in patients with a Finnish background, Oguchi disease (a type of stationary night blindness) in patients with a Japanese ancestry, Tay-Sachs or Gaucher disease in Ashkenazi Jewish patients (Jews from Eastern and Central Europe), or sickle cell trait or disease in patients with African, Southeast Asian or Mediterranean ancestry.
You should learn the characteristics of complex (multifactorial) disorders, monogenic disorders and chromosomal disorders. For example, for monogenic disorders, you should know the characteristics of autosomal dominant, autosomal recessive, X-linked, and mitochondrial (also known as cytoplasmic) inheritance patterns. Knowing these characteristics will allow you to recognize inheritance patterns in your patients via the family history and pedigree analysis.
6. Develop a referral network for genetic conditions.
Identify the genetic professionals in your geographic area and then establish an ongoing relationship with them. Learn how to refer patients to that professional. Also seek advice from a professional as you begin to acquire competency with genetics and ocular conditions. Find a genetic counselor or counselors in your area by going to the web site of the National Society of Genetic Counselors. (See table, page 64.) Once you access the web site, click on Find a Counselor.
Find a medical geneticist by going to the web site of the American College of Medical Genetics. Under ACMG Resources, click on Membership Directory.
You can also identify patient support groups for specific conditions using, for example, the Genetic Alliance web site.
7. Recognize the ethical, legal and social issues raised by genetic diagnosis.
You deal with issues of privacy and confidentiality on a daily basis. When you address genetic conditions, these issues take on a greater significance. You will need to learn how to obtain informed consent for genetic testing and to consider the possibility of genetic discrimination by employers or insurance companies. With the knowledge of a genetic disorder, patients may experience feelings of stigmatization, guilt or shame. In addition, genetic issues raise implications for the whole family. This is one of the reasons that the primary care optometrist is in a good position to handle genetic conditionstypically you know the patient and their family. Again, seek advice from the genetics professional(s) with whom you establish a relationship.
8. Learn how to locate genetic information and resources.
You need to develop your life-long learning skills. This includes learning how to use some of the excellent web-based resources available. (See table, page 64.) These sources are updated regularly. Visit each web site and explore what it has to offer.
When a patient raises a question about a genetic disease in the patients family or when you want to know more about a particular disease, a good source of information is the Online Mendelian Inheritance in Man (OMIM) web site. It is an authoritative, searchable source of information on human genetic diseases.
Another good resource is the Genetics and Your Practice web site. It has practical modules on Family Health and Social History, Genetic Testing and Screening and Referral to Genetic Services. It includes tools, forms, links and guidelines.
When you want to access the medical and ophthalmic literature, one of the major sites to use is the PubMed web site. It allows you to search the medical literature from 1966 to the present. This is an excellent way to keep up with new discoveries and new information on almost any medically-related topic, including ophthalmic genetics. It gives you access to abstracts of the articles and, in some cases, the full article. For any article, it allows you to find other related articles.
Primary care, pediatric and low-vision optometrists will play a crucial role in the integration of the new genetics into clinical practice.
By increasing genetics/genomics education in the schools and colleges of optometry and by increasing continuing education oppor- tunities for practicing optometrists, we can increase our skills in case recognition, diagnosis, management, patient education, and referral of genetics cases. And, by establishing and maintaining relationships with our colleagues who specialize in genetics, we can receive guidance as we increase our genetic competency and literacy. n
Dr. Wormington is an associate professor of biophysics and optometry at Pennsylvania College of Optometry (PCO), the staff biophysicist at the Light and Laser Institute at PCO, and on the clinical teaching staff at The Eye Institute at PCO.
- Collins FS. The Human Genome Project and the Future of Medicine. Ann N Y Acad Sci 1999 Jun 30;882:42-55.
- Bennett RL. The Practical Guide to the Genetic Family History. New York: John Wiley, 1999.
- Challa P. Glaucoma genetics: advancing new understandings of glaucoma pathogenesis. Int Ophthalmol Clin 2004 Spring;44:167-85.
- Wirtz MK, Samples JR. The genetic loci of open-angle glaucoma. Ophthalmol Clin North Am 2003 Dec;16:505-14.
- Tuo J, Bojanowski CM, Chan CC. Genetic factors of age-related macular degeneration. Prog Retin Eye Res 2004 Mar;23(2):229-49.
- Klein ML, Francis PJ. Genetics of age-related macular degeneration. Ophthalmol Clin North Am 2003 Dec;16:567-74.
- Hejtmancik JF, Kantorow M. Molecular genetics of age-related cataract. Exp Eye Res 2004 Jul;79(1):3-9.
- Reddy MA, Francis PJ, Berry V, et al. Molecular genetic basis of inherited cataract and associated phenotypes. Surv Ophthalmol 2004 May-Jun;49(3):300-15.
- Gilmartin B. Myopia: precedents for research in the twenty-first century. Clin Experiment Ophthalmol 2004 Jun;32(3):305-24.
- Schaeffel F, Simon P, Feldkaemper M, et al. Molecular biology of myopia. Clin Exp Optom 2003 Sep;86(5):295-307.
- Egan RA, Kerrison JB. Survey of genetic neuro-ophthalmic disorders. Ophthalmol Clin North Am 2003 Dec;16(4):595-605, vii.
- Klintworth GK. The molecular genetics of the corneal dystrophies current status. Front Biosci 2003 May 01;8:d687-713.
- Vincent AL, Rootman D, Munier FL, Heon E. A molecular perspective on corneal dystrophies. Dev Ophthalmol 2003;37:50-66.
- Daiger SP. Identifying retinal disease genes: how far have we come, how far do we have to go? Novartis Found Symp 2004;255:17-27; discussion 27-36, 177-8.
- Bird AC. What should a clinician know to be prepared for the advent of treatment of retinal dystrophies? Novartis Found Symp 2004;255:85-90; discussion 90-4, 177-8.
- Ocugene Glaucoma Genetic Test home page. URL: www.ocugene.com. (14 Sept 2004)
- Cohen CS, Allingham RR. The dawn of genetic testing for glaucoma. Curr Opin Ophthalmol 2004 Apr;15(2):75-9.
- Mackey DA, Craig JE. Predictive DNA testing for glaucoma: reality in 2003. Ophthalmol Clin North Am 2003 Dec;16(4):639-45.

