 |
An 85-year-old white male presented for an annual follow-up of cortical cataracts in both eyes. He did not feel his vision was appreciably worse than the year before. He had a history of asymmetric intraocular pressure (IOP) with the right eye always being slightly higher than the left. At his last eye exam one year earlier, IOP measured 21mm Hg OD and 18mm Hg OS. His medical history was significant for hypertension and hypercholesterolemia, for which he was taking diltiazem and rosuvastatin.
Upon examination, his best-corrected visual acuity measured 20/40 OD and 20/20 OS. Confrontation visual fields were full to careful finger counting OU. Motility testing was normal, and the pupils were equal, round and reactive to light; there was no afferent pupillary defect. The anterior segment exam was significant for nuclear sclerotic cataract and cortical cataract in both eyes, with the right eye worse than the left, and consistent with his visual acuity. Tensions by applanation measured 21mm Hg OD and 13mm Hg OS.
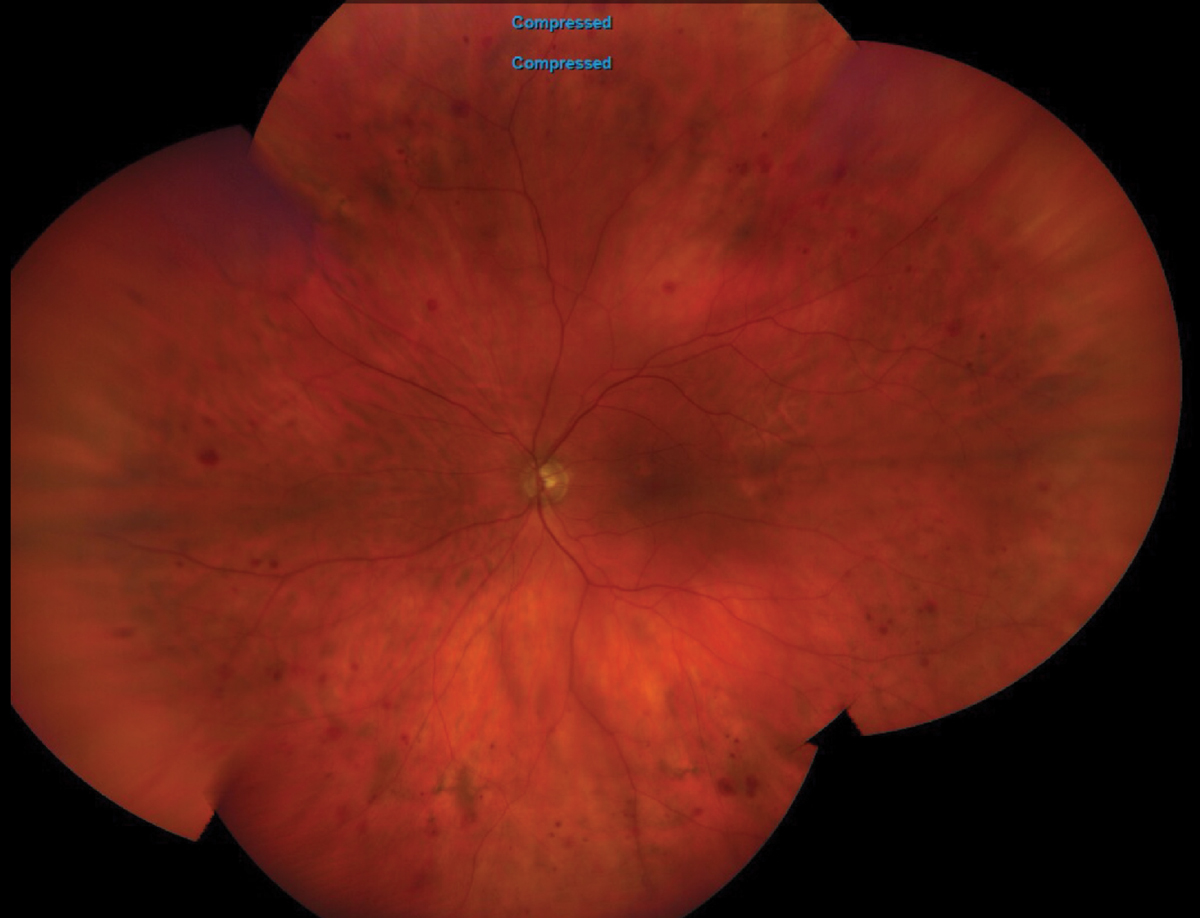
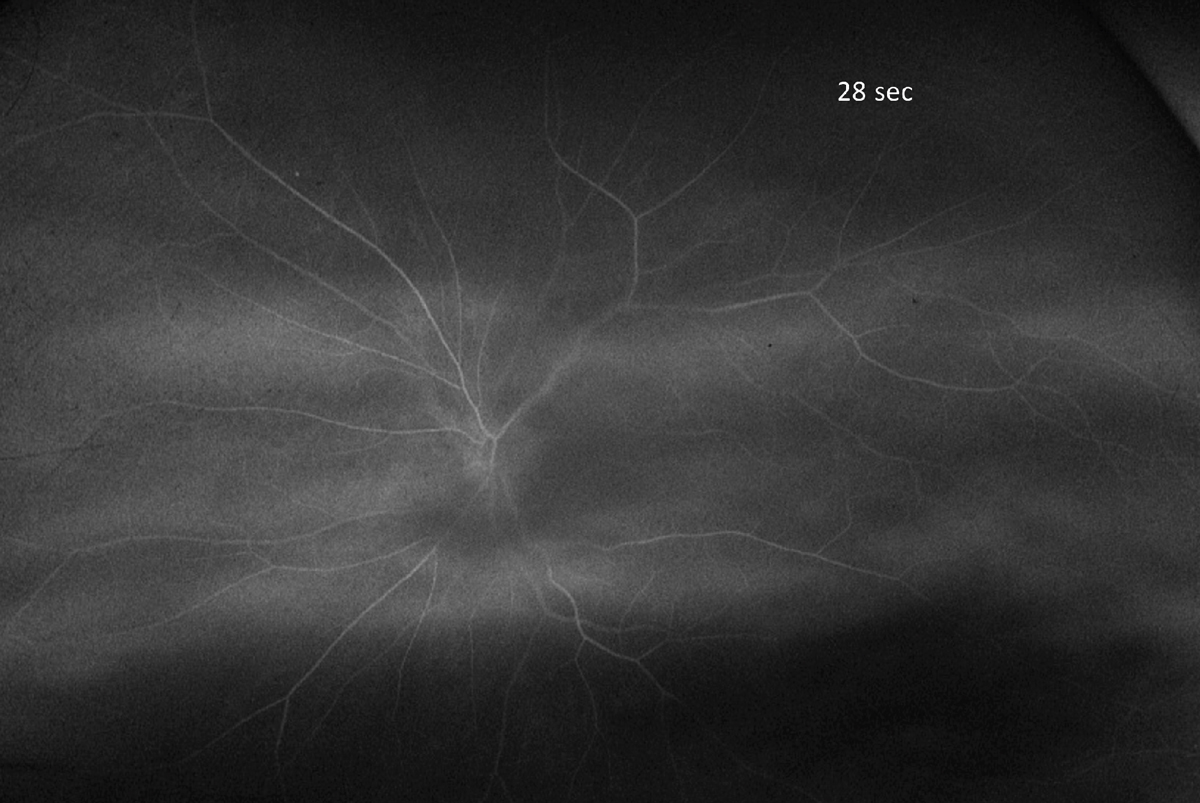
On dilated fundus exam, the cup-to-disc ratio measured 0.5 in each eye with temporal sloping. There was mild retinal pigmented epithelium mottling in the macula of each eye without subretinal fluid or choroidal neovascularization. The periphery of the right eye was normal, and there were scattered blot hemorrhages in the left eye (Figure 1). An OCT of the macula and retinal nerve fiber layer was normal, and an image of the fluorescein angiography (FA) at 25 seconds is available for review (Figure 2).
 |
|
Fig. 1. Here is a widefield view of the left eye of our patient. Note the peripheral retinal hemorrhages. What is the etiology? Click image to enlarge. |
Take the Retina Quiz
1. How would you interpret the FA?
a. Essentially normal.
b. Peripheral capillary nonperfusion.
c. Delayed arterial filling.
d. Occlusion of the central retinal vein.
2. What is the most likely diagnosis?
a. Early central retinal vein occlusion.
b. Venous stasis retinopathy.
c. Asymmetric nonproliferative diabetic retinopathy.
d. Ocular ischemic syndrome (OIS).
3. What additional testing is recommended?
a. Visual field.
b. OCT angiography.
c. Carotid artery studies.
d. MRI of the brain.
4. What additional findings would you expect to see with this condition?
a. Anterior segment neovascularization.
b. Macular edema.
c. Retinal neovascularization.
d. Posterior subcapsular cataract.
5. How should this patient be managed?
a. Careful observation.
b. Anti-VEGF injection.
c. Refer for consideration of endarterectomy.
d. All of the above.
For answers, see below.
Diagnosis
The presence of peripheral blot hemorrhages in the left eye was concerning, especially since they were not noted on his prior exam. The initial thought was that this is likely from an early or mild retinal vein occlusion, but, given his age, we also considered that the hemorrhages could be from ocular ischemic syndrome.
OIS is a rare condition caused by ocular hypoperfusion to the eye and orbit as a result of stenosis or occlusion of the common or internal carotid arteries, most commonly due to atherosclerosis.1,2 In most cases, a stenosis of 90% or more of the common or internal carotid artery on the ipsilateral side of the eye is usually seen. In 50% of the cases, the carotid artery is completely obstructed.
An FA was performed to determine if there was any delay in filling of the fluorescein dye, which we would expect to see if this were from OIS. Indeed, there was a delay; we didn’t see the choroidal filling until about 18 seconds (normal is 11 seconds) and we didn’t see the dye enter the central retinal artery until about 28 seconds. The normal arteriovenous transit time is also approximately 11 seconds.
Based on the clinical and FA findings, it was recommended that our patient have a complete work-up by his cardiologist, including carotid artery studies. We also tried to elicit any history of transient ischemic attach-like symptoms or other indications of a stroke. He denied any symptoms of transient visual loss or other stroke-like symptoms. In fact, he said he was pretty healthy and felt fine.
The patient was seen by his cardiologist and had carotid duplex scanning done. The results showed that there was a near occlusive atherosclerotic plaque at the left common carotid artery bifurcation and proximal bulb with severe high-grade stenosis of at least 70% to 95%. There was also extensive atherosclerotic plaque in the right common carotid bifurcation and bulb with 50% to 69% stenosis proximal right internal carotid artery. The report concluded that there was high-grade stenosis of both external carotid arteries with reversal of flow in the left external carotid artery and high velocity stenosis at the origin of the left vertebral artery. Given these results, we were able to establish a definitive diagnosis of OIS.
 |
|
Fig. 2. Here is a frame of the FA at 28 seconds. Is this normal? Click image to enlarge. |
Discussion
The exact incidence of OIS is unknown. The mean age of patients is 65 years, and men are affected twice as often as women.1,2 This is likely attributed to the higher incidence of cardiovascular disease in males. In 20% of cases, the involvement is bilateral. Vision loss is seen in up to 90% of patients due to retinal ischemia and/or secondary glaucoma.1 Fortunately, our patient had excellent visual function.
He did not have glaucoma but, interestingly, patients with OIS can have either elevated IOP from anterior segment neovascularization or low IOP as a result of ciliary body shutdown from the ischemia. In fact, iris or angle neovascularization can be seen in up to 66% of eyes with OIS and may be the only presenting sign of the condition.1 Luckily, our patient did not have any anterior segment neovascularization.
Other findings commonly seen with OIS—in addition to retinal hemorrhages and anterior segment neovascularization (ASNV)—include orbital pain or a dull ache in about 40% of patients, likely from orbital hypoxia, and anterior chamber flare when ASNV is present.1 Other posterior segment findings may include narrowed arteries and dilated veins, which was not obvious in our patient.
All of this was explained to our patient, and the cardiologist even discussed the option of surgical intervention with endarterectomy. In the end, our patient declined to have any treatment beyond routine follow-up on a regular basis. He was seen one year later and was still functioning well. The acuity in the left eye had dropped to 20/25 and the retinal hemorrhages were still present. He still had asymmetric IOP of 22mm Hg OD and 14mm Hg OS. He reported that he is doing well and living a productive life, including playing golf on a regular basis.
Retina Quiz Answers
1: c, 2: d, 3: c, 4: a, 5: c
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Terelak-Borys B, Skonieczna K, Grabska-Liberek I. Ocular ischemic syndrome–a systematic review. Med Sci Monit. 2012;18(8): RA138-44. 2. Brown GC, Magargal LE. The ocular ischemic syndrome. Clinical, fluorescein angiographic and carotid angiographic features. Int Ophthalmol. 1988;11(4):239-51. |

