Corneal reshaping is a rapidly progressing and increasingly popular modality worldwide and has demonstrated success in myopia reduction with patients as young as age 7.1-3
There have been some reports of adverse reactions in patients during corneal reshaping (see Corneal Reshaping and Microbial Keratitis, page 60).4-11 But, with careful patient education and compliance, these complications are avoidable.
Here, well look at some of the latest designs and fitting pearls for corneal reshaping and who the best candidates are for this modality.
Whos a Candidate?
Most patients with -4.50D or less myopia are suitable candidates for corneal reshaping. Patients often experience a myopic reduction of 1.00D to 2.00D the first night.12
Many O.D.s limit eligible patients to the non-presbyopia age group, although monovision corneal reshaping (i.e., undercorrecting one eye) is occasionally prescribed. Presbyopic corneal reshaping designs show promise, according to recent research.13
If youve just introduced corneal reshaping into your practice, you might want to start with the -1.00D to -2.00D myopic patient to gain confidence with this process. Also, start with young adults who are either non-contact lens or soft contact lens wearers and have no more than -1.50D of corneal cylinder (preferably not limbus-to-limbus). Corneal reshaping may result in a 50% reduction of central corneal toricity.14 Patients with against-the-rule or irregular astigmatism are not good candidates.15
You can prescreen potential patients by phone. When patients schedule an appointment, you (or your staff) can ask them about any known refractive error and current lens wear. Make sure that patients who are good candidates for corneal reshaping understand that this is a temporary process that requires retainer lens wear at night and compliance with the wearing schedule and care regimen.
Spherical gas permeable (GP) lens wearers must discontinue lens wear for at least four weeks before being fit with ortho-K lenses. Expect more lens exchanges and variable topography maps with these patients, even if they discontinue GP lens wear as recommended.16
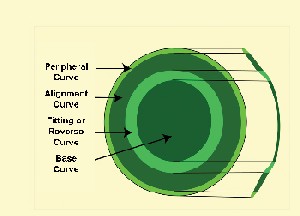
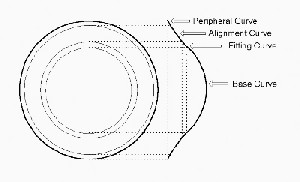
The lens designs we commonly use for ortho-K have at least four zones: the base curve; the secondary, or reverse, curve, which is often 3.00D to 5.00D steeper than the base curve; an intermediate alignment or fitting curve, which parallels the mid-peripheral cornea; and a peripheral curve radius, which is often slightly steeper than conventional designs, resulting in less peripheral clearance.17 The optical zone is often 6mm (it will be less in certain designs for higher refractive errors). Regardless of which design you select, fitting and follow-up care must be consistent.
Some designs use the Jessen factor, which is based simply upon lacrimal lens power changes. For example, if the patients spherical refractive error is -3.00D, you would select a base curve radius approximately 3.50D to 3.75D flatter than K to result in a refractive error of +0.50D to +0.75D. This is an ideal power to allow for regression of refractive error during the day. So, if the patient has keratometry readings (or simulated K values) of 43.75 @ 180 or 44.50 @ 090 and a prescription of -3.75 -0.75 x 180, you would use a base curve radius of 40.00D for +0.75D. A corneal topographer is important in the pre-fitting, fitting and follow-up of all corneal reshaping patients.
A bulls-eye lens-to-cornea fitting relationship with limited movement upon blinking and zones of less clearance and more clearance should be present (figure 1). Centration is extremely important, as a decentered lens will result in a decentered treatment zone and symptoms of glare, ghost images and variable vision.
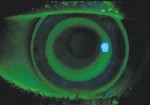 |
| 1. The fluorescein pattern shows a bulls-eye lens-to-cornea fitting relationship. |
Assess corneal topography, unaided vision and refractive error. The difference map should show a well-centered bulls-eye pattern (figure 2). If the topography is inconclusivethat is, not entirely the desired bulls-eye pattern but not excessively flat (smiley-face) or steep (central island)have the patient return three days after the initial fit to further assess the lenses. On average, it takes 10 days to achieve a stable endpoint.18
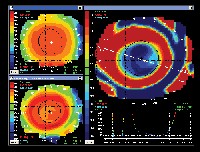 |
| 2. This representative difference map shows a well-centered bulls-eye pattern. Courtesy: Precision Technology Services |
|
Corneal Reshaping and Microbial Keratitis Use a corneal topographer. This is invaluable in patient selection, fitting and follow-up care. Corneal topography can determine a decentered corneal apex or the presence of subclinical keratoconus; both of these rule out corneal reshaping. Topography also can help you determine corneal eccentricity; studies have shown that the more corneal eccentricity present, the greater the potential myopia with corneal reshaping.9 |
The FDA has approved these lenses for corneal reshaping:
Paragon CRT (Paragon Vision Sciences). The CRT, which stands for Corneal Refractive Technology, was the first lens approved for overnight corneal reshaping. This lens consists of a 6mm central treatment zone, a 1mm wide return zone of variable depth, a tangent curve, a landing zone and an ellipse edge profile. Do not allow the terminology to confuse you, as this design is not complicated to fit. Laminated lens selection and problem-solving cards are available from Paragon.19
This design uses a diagnostic lens fitting approach. Paragon has a 100-lens CRT Diagnostic Dispensing System with a range of base curves, return zone depths and landing zone angles selected to result in the ability to dispense from inventory in the majority of cases.
BE Retainer (Precision Technology Services). The topography-based system uses eccentricity value, apical radius and horizontal visible iris diameter to determine the recommended lens design (figures 3 and 4). Any changes in lens design depend upon the resultant topography map (bulls-eye, smiley face or central island).
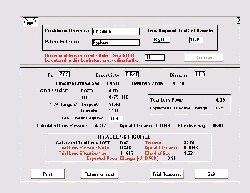 |
| 3. The topography software printout for the BE Retainer shows the recommended trial lens, taking apical radius, corneal eccentricity and effective sag into consideration. Courtesy: Precision Technology Services |
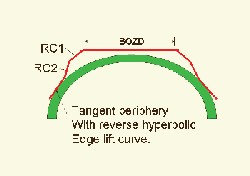 |
| 4. The BE Retainer lens is a topography-based system. Courtesy: Bausch & Lomb |
 |
| 5. The Contex E-System lens design most often has an optical zone of 6.0mmbut it can vary from 5.0mm to 8.0mmand the peripheral curve is aspheric. Courtesy: Bausch & Lomb |
 |
| 6. The Dreamlens features a four-zone reverse geometry lens design. Courtesy: Bausch & Lomb |
 |
| 7. The Emerald lens design features four zones and a standard power of +0.75D. Courtesy: Bausch & Lomb |
| Corneal Reshaping Lens Designs/Certification Bausch & Lomb Vision Shaping Treatment: www.bausch.com/us/ resource/visioncare/vst/index.jsp BE Retainer (Precision Technology Services): www.beretainer.com Contex OK E-System (Contex): www.oklens.com DreamLens (DreimLens Inc.) www.dreimlens.com Emerald (Euclid Systems Corp.): www.euclidsys.com Paragon CRT (Paragon Vision Sciences): www.paragoncrt.com |
Dr. Bennett is executive director of the Gas Permeable Lens Institute and is co-chief of the contact lens service and director of student services at University of Missouri-St. Louis College of Optometry.
1. Walline JJ, Rah M, Jones LA. The Childrens Overnight Orthokeratology Investigation (COOKI) pilot study. Optom Vis Sci 2004 Jun;81(6):407-13.
2. Reim TR, Lund M, Wu R. Orthokeratology and adolescent myopia control. Contact Lens Spectrum 2003;18(3):40-42.
3. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res 2005 Jan;30(1):71-80.
4. Young AL, Leung AT, Cheng LL, et al. Orthokeratology lens-related corneal ulcers in children: a case series. Ophthalmology 2004 Mar;111(3):590-5.
5. Hutchinson K, Apel A. Infectious keratitis in orthokeratology. Clin Exp Ophthalmol 2002 Feb;30(1):49-51.
6. Wilhelmus KR. Acanthamoeba keratitis during orthokeratology. Cornea. 2005 Oct;24(7):864-6.
7. Swarbrick H, Watt K. Microbial keratitis in orthokeratology: The worldwide perspective. Presentation at the 2005 Global Orthokeratology Symposium, Chicago, July 2005.
8. Cho P. Microbial flora of tears of ortho-k patients and microbial contamination of contact lenses and contact lens accessories. Presentation at the 2004 Global Orthokeratology Symposium, Toronto, July 2004.
9. Mountford J. An analysis of the changes in corneal shape and refractive error induced by accelerated orthokeratology. Int Contact Lens Clin 1997;24:128-143.
10. Herzberg CM. Improved efficacy of eye gel lubricants vs. rewetting drops in Ortho-k. Presentation at the 2005 Global Orthokeratology Symposium, Chicago, July 2005.
11. Rah M. Personal communication. July 2005.
12. Sridharan R. Response and regression of the cornea with short-term orthokeratology lens wear. Masters thesis, University of New South Wales, Sydney, Australia, 2001.
13. Legerton J. Corneal Refractive Therapy for hyperopia and presbyopia. Presented at the Global Orthokeratology Symposium, Toronto, July 2004.
14. Mountford J. Advanced orthokeratology: Part 2: Patient selection and trial fitting. Optician 2002;224(5867):26-37.
15. Rinehart JM, Bennett ES. Orthokeratology. In Bennett ES, Hom MM. Gas Permeable Contact Lenses (2nd ed.), St. Louis, MO, Elsevier, 2004:424-483.
16. Subramaniam SV, Bennett ES, Morgan B, Lakshrimnarayanan V. Comparison of overnight orthokeratology in RGP and non-RGP wearers. ARVO Abstract #3713, 2003.
17. Bausch & Lomb. A Guide to Overnight Orthokeratology, www.bausch.com/us/resource/ visioncare/orthok/guide_to_orthok.pdf. Accessed August 2005.
18. Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci 2003 Jun;44(6):2518-23.
19. McCampbell K, Bennett ES, Rah M. Corneal reshaping made easy with the CRT lens. Contact Lens Spectrum 2004;19(10):30-37.

