Contact lenses are a significant part of the average optometric practice, comprising an estimated one-third of profits.1 Yet, with an increasing number of patients moving to contact lens wear, the potential for dissatisfaction—and patient dropout and loss of revenue—is of greater concern than ever. On average, one-fourth of contact lens patients cease wearing lenses, with the primary reasons being discomfort and dryness.2
Looking to the Past
In the last few years, we have seen the introduction of game-changing technologies that have challenged the way we think about contact lens comfort and the way we correct our patients’ vision needs. In our Review of Cornea & Contact Lenses column, Derail Dropouts, we have examined the ways in which we can reduce contact lens dropouts since we began the column in 2008. While not a comprehensive list, some of the major topics discussed include:
• Improve Care Compliance. Patient non-compliance with contact lens care is a significant, ongoing concern. Rates of non-compliance—which is defined as failure to adhere to lens replacement schedules; inadequate lens cleaning and storage practices; and exposure to water or other liquids that may harbor bacteria—historically range from 40% to 91%.3 Failure to comply can lead to severe complications, including corneal ulcers and sight-threatening bacterial or fungal infections.
So, how do you determine what your patients are doing to care for their lenses? The answer is fairly simple: ask them to bring their contact lens cases, solutions and any other care products, as well as any drops they may be using, into the office. Seeing them firsthand gives you the opportunity to educate patients on proper lens care, if needed, and intervene with appropriate clinical solutions if necessary. Interventions might include refitting them into a daily disposable lens to alleviate risk of infection from mishandling, or suggesting an alternate solution that may better interact with the lens material.
• Consider the Modality. From daily disposable contact lenses to two-week, one-month and the quarterly or yearly replacement schedules, today’s contact lens wearers have many options when choosing a lens modality. Ultimately, however, eye care practitioners are responsible for guiding the selection of a proper contact lens modality, material and solution combination to ensure lens wear success. For patients who are successful extended wearers, high oxygen permeable materials are a good choice, as they ease oxygen transmission to maintain ocular surface health. Those who have difficulty complying with lens care regimens, however, may benefit from daily disposable lenses.
• Identify Silent Sufferers. Many contact lens wearers will not tell you about their contact lens discomfort. Searching for objectivity in their subjective responses to a series of questions can help expose a significant decline in comfort that might occur throughout the day.
Ask patients to rate their comfort on a scale from zero to 10 approximately five to 10 minutes after the lenses have settled on their eyes in the morning, with zero being the least comfortable and 10 being the most comfortable. Also, ask them to rank the comfort of their lenses at the end of the day, about five to 10 minutes prior to removing the lenses in the evening. If there is a drop in this number, it is up to you to determine why.
The reasons are usually multiple, and can include poor compliance with care and replacement regimens, leading to increased deposits on the lens, which decreases comfort. Certain ocular surface conditions also have a significant effect on comfort.
• Discuss Ocular Allergies. Eyes experience significant differences in the type of allergic responses. Vernal keratoconjunctivitis and atopic keratoconjunctivitis are often relatively easy to identify, as these presentations typically include itching, photophobia, burning and tearing.
The first and most important step to managing lens dropout due to allergies is identifying those who have seasonal allergies and asking them the right questions. Patients typically experience intermittent, rather than constant, discomfort throughout the year, so be sure to evaluate patients several times annually.
Possible solutions include medical management, switching to a more frequent replacement schedule or peroxide cleaning and disinfecting systems.
• Don’t Ignore Dry Eye. We have looked at this common disease in great detail throughout the years. Contact lenses introduce a specific challenge to the ocular surface, as its health must remain balanced against the interaction of the contact lens and the eye. A healthy tear film provides consistent, comfortable vision for individuals who are not contact lens wearers, as the interaction between the eyelids and the tear film is appropriately balanced in healthy individuals.
 | |
| Don’t overlook the eyelids. They can be the root cause of contact lens discomfort. |
Even if the quality of the tear film is compromised, the ocular surface may still be able to provide a symptom-free experience for the individual. Introducing a contact lens to a compromised tear film, however, may lead to dry eye symptoms in individuals who might otherwise have virtually no symptoms, or exacerbate preexisting symptoms.
The eyelids are often overlooked as a potential source of contact lens discomfort. Many eye care providers are relatively quick to change the type of contact lens when a patient complains of discomfort, but this may not treat the underlying cause of the problem. By addressing the issues that may compromise the health of the ocular surface, however, you can increase your chances of improving comfort in lens wearers. Ensuring healthy meibomian gland physiology is critical, as is addressing anterior blepharitis and maintaining the aqueous layer of the tear film.
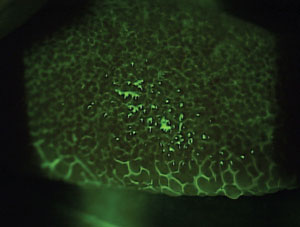
Incorporate a well-structured examination process for contact lens wearers that includes the use of vital dyes and a systematic assessment of the ocular surface. Identify conditions, such as lid wiper epitheliopathy, that can affect healthy lens wearer, to help improve contact lens comfort.
• Consider Lens Characteristics. It is important to consider new materials and polymers that may improve contact lens comfort for patients. New materials designed for better comfort have been introduced in the last several years, including delefilcon A, samfilcon A and somofilcon A.
These designs and materials may provide additional comfort to individuals on the verge of dropping out of lens wear, especially patients whose unique visual demands are a limiting factor.
For astigmatic patients who are typically less than 2.50D, a number of disposable lens choices are readily available in diagnostic fit sets. For those whose astigmatism is greater than 2.50D, specialty soft lens designs can be custom-made through a lathing process that offers a higher level of astigmatic correction.
Traditional gas permeable (GP) lenses, including back surface toric and bitoric lenses, provide a remarkably high level of visual quality because of the high quality of the lens optics, the tear film that can be produced between the posterior surface of the lens and the cornea, and also the stability added to a lens when a toric surface is created on the posterior surface of the lens.
However, some patients may have a difficult time wearing small diameter GP lenses comfortably. For these patients, hybrid lenses can offer the visual benefits of a standard GP with the added benefit of being surrounded by a soft lens skirt to minimize lens edge awareness. Scleral lenses, while traditionally reserved for patients with irregular corneas, are another good option for those with high levels of ametropia, specifically astigmatism that has failed with more traditional technologies.
Presbyopic patients can be especially hard to fit, as they require both distance and near correction that is different and distinct in magnitude. Most of the lenses (other than a translating GP lens design) are based on simultaneous vision designs, which simply focus both the distance and near optics on the retina at the same time.
Significant advances have provided clinicians more options to fit their presbyopic patients with daily disposable multifocal contact lenses; however, with all of the advances in lens technologies, there is still a segment of the presbyopic population that cannot wear multifocal contact lenses. The reason behind this is likely multifactorial and may include decreasing pupil size with increasing age; problems adjusting to simultaneous vision; and improper optical alignment of the lens powers with a patient’s line of sight.
Additionally, relevant to the topic of comfort, the increase in dry eye that begins to occur around the time of prescription development may also play a role. All of these factors become more challenging with increasing higher add powers. Although lens technologies may address some of these concerns, other technologies are still under investigation to improve these characteristics.
Moving Onward
Our Review of Cornea & Contact Lenses column has traditionally focused on helping you prevent patient’s from dropping out of lens wear—in effect, plugging the leaky bucket and helping to maintain the wearers you do have. Beginning with the September issue, however, we will be shifting the focus of our column to one that discusses ways to increase the population of contact lens wearers in your practice. We will continue to update readers on new lens technologies, ocular surface disease treatments and other therapeutics that ease the introduction of contact lenses to new patients. Some of these new topics include:
• Specialty Contact Lenses. Patients who require medically necessary contact lenses, including those with keratoconus and post-traumatic corneas, irregular or highly astigmatism and post-refractive surgery, often require more time and energy to fit. The time involved varies with the condition, depending on the degree of corneal irregularity. However, satisfying these patients can be extremely rewarding, as they often have been unsuccessful in other modalities.
• Pediatric Daily Disposable Lenses. Because this modality offers patients the convenience of a fresh lens each time without the hassle of cleaning or a replacement schedule, children interested in part-time wear—for example, during physical activity—may represent an underserved but valuable market.
• Research and Innovation. In health care, research is critical to the growth and acceptance of new materials, treatments and protocols. Breakthroughs within the contact lens field may change your approach as an eye care practitioner, including the way you fit a particular group of patients or how you use a specific medical device. Contact lens material innovation may improve ocular health, treat diseases and improve comfort. Also, new optical designs aim to improve visual outcomes for a variety of refractive errors, including astigmatic and presbyopic patients.
• Alternative Uses. There are some common alternative uses for contact lenses, including bandage contact lenses for the treatment of ocular surface disease. More will be developed and may become mainstream in many of our practices.
• Digital Device Use. Now more than ever, digital devices are an integral part of our daily lives. Many patients spend their workdays in front of a computer, supplemented by use of handheld devices such as smartphones or tablets throughout the day. Contact lens wear is complicated by a decreased blink rate and visual fatigue when using these devices, and it is imperative you take the time to address this clinically.
In contact lens practice, we have focus on “change management,” i.e., adapting our approach to contact lens care as the patient’s visual needs and ocular health change over time. Whether it’s new materials, modalities or technologies, it is imperative we offer the best option for our patients’ visual well-being.
We look forward to writing about these topics in our new column, Practice Progress, debuting in the September issue of Review of Cornea & Contact Lenses, which will focus on growing—not just retaining—the contact lens patient base in your clinics.
Dr. Brujic is a partner of Premier Vision Group in Ohio. He practices full scope optometry with an emphasis on ocular disease management of the anterior segment, contact lenses and glaucoma.
Dr. Miller is a partner in a private practice in Powell, Ohio and an adjunct faculty member for the Ohio State University College of Optometry. Dr. Miller has lectured on contact lenses, myopia, dry eye, allergic conjunctivitis and practice management.
1. Nichols Jason J. 2014 Annual Report: Contact Lenses 2014. Contact Lens Spectrum. Jan. 2015;(30):22-27.2. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Corena. 2007 Feb;26(2):168-74.
3. Robertson DM, Cavanagh HD. Non-compliance with contact lens wear and care practices: a comparative analysis. Optom Vis Sci. 2011 Dec; 88(12):1402-8.

