 A 26-year-old white female presented for an eye examination with a chief complaint of bilateral visual acuity deterioration during the last five years.
A 26-year-old white female presented for an eye examination with a chief complaint of bilateral visual acuity deterioration during the last five years.
She explained that other eye doctors had examined her, but failed to diagnose a specific problem. The patient said that her vision had not been the same since her college internship in Holland.
Her systemic history was unremarkable and her ocular history was noncontributory. She reported no known allergies.
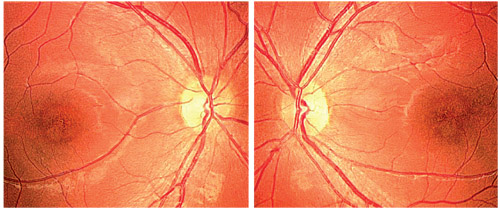
1, 2. This 26-year-old patient
reported bilateral acuity deterioration since returning from her
college internship in Holland several years ago (O.D. left, O.S. right).
Her best-corrected acuity measured 20/60 O.D. and 20/300 O.S. at distance and near. Her color vision was altered in both eyes, without a specific anomalous orientation. There was no relative afferent pupillary defect.
Amsler grid testing uncovered relative central deficits in both eyes. Additionally, the patient exhibited a positive Watzke-Allen sign O.U., which indicated the presence of macular discontinuity. Refraction uncovered mild hyperopia, with no visual improvement in either eye.
The anterior segment examination was completely normal. Intraocular pressure measured 14mm Hg O.U. The dilated fundus examination demonstrated significant posterior pole findings in both eyes (figures 1 and 2).
Your Diagnosis
How would you approach this case? Does this patient require any additional tests? What is your diagnosis? How would you manage this patient? What’s the likely prognosis?
Discussion
Additional tests included Amsler grid, brightness screening, rechecking for a relative afferent pupil defect with a neutral density lens filter, frequency doubling perimetry (FDP) and laser interferometry. Upon further questioning, the patient revealed an extensive history of tanning bed use.
The diagnosis in this case is bilateral ultraviolet light-induced maculopathy, which resulted from multiple sessions in a tanning booth. The patient recounted that the tanning salon owner in Holland did not issue her sunglasses. The patient admitted to opening her eyes on at least five occasions while inside the tanning bed.
Irreversible retinal damage is the most serious consequence of unprotected sunlight exposure.1 Retinal light injury occurs when incident light rays enter the eye almost parallel to the unprotected visual axis.2 Factors that influence the composition of the light spectrum on the retina include not only the environment, but light reflection from the cornea, as well as UV absorption and filtering by the cornea, aqueous, lens and vitreous.1
This patient’s unique presentation is comparable to documented cases of solar retinitis secondary to gazing at the sun or a solar eclipse. The cellular correlates of solar retinopathy include neuronal apoptosis as well as glio-vascular responses. Cellular apoptosis is an irreversible process that can result in permanent visual impairment.3
UV-emitting lamps are extremely intense and can cause severe damage to the skin and eyes.4 Once phototoxicity occurs, there is no formal treatment strategy. Induced macular holes may be surgically repaired, but the final prognosis depends on ocular tissue health.
While there is no restorative treatment option, we elected to monitor our patient for the development of choroidal neovascularization. In the future, low vision rehabilitation services might offer hope for an improved condition of life.
Thanks to Shaeleen Blum, O.D., of Washington D.C. for contributing to this case.
1. Verma L, Venkatesh P, Tewari H. Phototoxic retinopathy. Ophthalmol Clin North Am. 2001 Dec;14(4):601-9.
2. Sliney DH. Ocular injury due to light toxicity. Int Ophthalmol Clin. 1988 Fall;28(3):246-50.
3. Thanos S, Heiduschka P, Romann I. Exposure to a solar eclipse causes neuronal death in the retina. Graefes Arch Clin Exp Ophthalmol. 2001 Oct;239(10):794-800.
4.
Gallagher RP, Lee TK. Adverse effects of ultraviolet radiation: a brief review. Prog Biophys Mol Biol. 2006 Sep;92(1):119-31.

