|
JOHN MURPHY, Senior Editor; and |
Of all ocular conditions, presbyopia is perhaps the only one that affects everyone who lives past age 40. Given the aging of the population, its no wonder that the National Eye Institute has made presbyopia one of its research priorities, as have individual researchers.
For nearly 150 years, weve accepted Hermann L.F. von Helmholtzs theory of accommodation: That the unaccommodated crystalline lens remains under tension by the zonules and the ciliary muscle, pulling the lens toward the sclera, and giving the lens a flatter shape. To accommodate, the ciliary muscle tightens and extends toward the lens. This relaxes the zonular fibers, which allows the lens to return to a slightly more convex shape. The surface of the lens now has increased optical power to allow the eye to focus on near objects.
Yet, this theory also has been challenged. Today, two schools of thought predominate about what causes presbyopia. One, that presbyopia results from a hardening of the lens and stiffening of the lens capsule with age so that the lens cannot change shape. And two, that the ciliary muscle, as it ages, loses its ability to contract and change its configuration.
However, both are happening simultaneously. Does one cause the other? Some researchers feel that both mechanisms are at play, while others are more inclined to implicate the crystalline lens. Meanwhile, one researcher suggests that the real cause of presbyopia is the continued growth of the lens. Their research may one day lead to new treatments.
Something of a Stretch
It has been long thought that sclerosis of the lens is one important factor in the onset of presbyopia. Specifically, the human lens hardens and becomes less pliable with age, and gradually loses its ability to undergo accommodative changes. How does the lens age? How does that aging process affect the progression of presbyopia?
Adrian Glasser, Ph.D., of the University of Houston College of Optometry, and Melanie C.W. Campbell, Ph.D., of University of Waterloo (Ont.) School of Optometry, wanted answers. So, Dr. Glasser designed a mechanical stretching apparatus with which to study lenses of human eye bank eyes.
With mechanical stretching, the younger human lenses underwent optical changes comparable to the accommodative amplitude in a young human eye, but the older lenses failed to undergo any accommodative change. Drs. Glasser and Campbell also found substantial optical changes with increasing age and during accommodation.1
The researchers found that removing the lens capsule from each lens also caused changes in focal length, more so for the younger than the older lenses. The researchers say that the changes in focal length are due to nonsystematic changes in the lens curvatures.2
The studies demonstrate that the lens loses its accommodative ability with age and that it is possible to explain the progression of presbyopia in terms of age-related lens changes. And those kinds of mechanical stretching experiments are really independent of changes in zonular elasticity, or changes in the ability of the ciliary muscle to contract, for example, because were mechanically bypassing those parts of the normal accommodative system, Dr. Glasser says.
He does acknowledge, however, that there may be other age-related changes occurring in the eye and accommodative apparatus. But what it says, he adds, is that the lens is a fundamental limiting factor in the ability of the presbyopic human eye to undergo accommodative changes.
Combined Factors
Based on years of research with rhesus monkeys, Paul L. Kaufman, M.D., of the University of Wisconsin, believes that a combination of the two factorssclerosis of the lens and changes in the ciliary musclemay be at work.3 There are definitely changes in the lens and lens capsule that make it more difficult for the lens to move as we get older, he says.
He also has observed a decrease in movement of the ciliary muscle with age. However, Dr. Kaufman suggests that the real change may be a stiffening of the connective tissue that attaches the muscle to the wall of the eye. So, although the muscle contracts, it cannot move effectively enough to allow the lens to change shape.4
Nonetheless, he is reluctant to say that either sclerosis of the lens or stiffening of the ciliary muscle causes the other. Theoretically, either by itself could account for presbyopia, but theyre both happening simultaneously, or concurrently at least, he says.
Dr. Kaufman has studied presbyopia in iridectomized rhesus monkeys over their entire life span. Rhesus monkeys accommodate in a similar fashion both anatomically and physiologically to humans, and the rate of decline of accommodation in both species relative to their life span is identical.5,6
In his work with the rhesus monkeys, Dr. Kaufman, along with Dr. Glasser, observed that the ciliary body and the lens equator moved away from the sclera during accommodation.7 This is consistent with the Helmholtz theory of accommodation.
An Aging Lens


Proof of Helmholtzs theory: A 30-year-old eye at infinity (top left) and the same lens at 7.00D accommodation (top right). Note that the accommo-dated lens is thicker, more sharply curved and with a shallower anterior chamber. Compare that to a slightly emmetropic 69-year-old presbyopic lens (right), which is even thicker, darker, more curved and has a shallower anterior chamber. Courtesy: Jane F. Koretz, Ph.D.

Jane F. Koretz, Ph.D., a professor of biology at Rensselear Polytechnic Institute in Troy, N.Y., challenges that presbyopia is a function of the aging crystalline lens, not the weakening ciliary muscles or other factors.
The ciliary muscle, like any well exercised muscle, will continue to perform throughout life. The lens, however, ages and loses its ability to accommodate. Dr. Koretz says this loss happens through two distinct processes: the lens gradually thickens both posteriorly and anteriorly, and it undergoes biochemical changes over the years.
Dr. Koretzwho collaborates on research with Dr. Kaufmanstudied more than 100 emmetropes ages 18-70 and determined that the lens gradually grows thicker at a constant rate throughout life.8,9
The lens is made of basically the same type of cells as the skin, Dr. Koretz explains. But unlike the skin, which sloughs off cells daily, the lens never loses cells. Instead, new cells are added to the outside of the lens, with the oldest cells in the center. (Perhaps the new outer cells serve to protect the older inner cells, which may be more susceptible to degradation, Dr. Koretz theorizes.) This thickening of the lens only occurs posteriorly and anteriorly; its equatorial diameter does not increase.
As the lens thickens, both sides take on a shaper curve. However, the posterior side stays in the same place, so the front and center of the lens move forward. This makes the anterior chamber shallower.10 Mechanically, it becomes harder to manipulate, Dr. Koretz says. Accommodation decreases.
Meanwhile, the proteins in the lens cells are aging and losing their ability to refract perfectly. Handily, the increasing curvature of both lens surfaces appears to be natures way of negating the cells loss of refractive ability.11 The sharper curvature of the lens surface compensates almost exactly for the loss of refractive power of the material that the lens is made of, Dr. Koretz says.
The lens seems to develop and age in the same way in all normal human eyes regardless of visual acuity, she says. So although presbyopia manifests in those in their 40s, loss of accommodation may begin as early as age 18.
Once the lens loses its ability to focus, the rate at which the lens proteins age seems to speed up. Thats why people start having problems at night with glare, at the same age range that theyre having trouble getting adjusted to reading glasses, Dr. Koretz says.
She theorizes that a lot of changes in the viscoelastic properties of the lens are the result of presbyopia, not just the cause of it. This is on top of stiffening due to thickening as well as to cellular changes throughout life. Dr. Koretz suspects that the movement of the accommodating lens helps agitate the cytoplasm in the cells, which are jam-packed with protein. As the lens loses accommodation, the movement of the lens slows down, and the lack of agitation leads the proteins to essentially stagnate. This, she thinks, accelerates the stiffening of the lens.
Restoring Accommodation National Panel: For Presbyopes, Surgery is No PAL
Dr. Koretz predicts that these observations may aid in the development of a malleable artificial lens, specifically a deformable intraocular lens for cataract patients that would restore their ability to focus. Within 10 years, Dr. Kaufman foresees IOLs that will restore at least some accommodative ability.
Several such lenses are either under development or undergoing clinical testing, including an IOL from Quest Vision, the Accommodative 1CU (HumanOptics) and the CrystaLens Model AT-45 (C&C Vision). Researchers are implanting these IOLs into human eyes.
While preliminary investigations show that these lenses may indeed be capable of restoring accommodation, Dr. Glasser says that objective measurements are essential to prove whether they really can restore accommodation.
In his own studies on rhesus monkeys, Dr. Kaufman has found that some movement of the ciliary muscle remains, even in the oldest animals. Assuming one can translate that to the human, there is some movement left to work with, he says.
Thats important, because an accommodating IOL would not be effective without the elasticity of the capsule and muscle. Dr. Kaufman further points out that it may only be necessary to restore 3.00D to 6.00D of accommodation, depending on a patients individual tasks.
Another important consideration: An intact capsule is more elastic than one with a doughnut hole. If an artificial lens were to cause opacity of the lens capsule, and you were to perform a YAG laser capsulotomy, the lens capsule would become less elasticand less able to drive movement of the IOL, degrading lens performance.
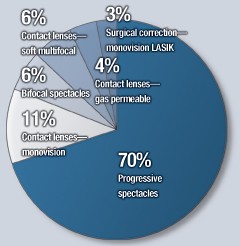
Among treatment options for presbyopia, surgical correction might be intriguing to read about, but optometrists overwhelmingly give the nod to spectacle correction when it comes to choosing an option for presbyopic patients.
Thats the clear message delivered in this months National Panel, Doctors of Optometry, survey: About 19 out of 20 doctors responding to our survey say that their favorite corrective option for presbyopes is spectacles.
Its easy to understand why: better binocularity, lower cost, easier to use, better vision at all distances, more options, and no health risk.
Meanwhile, only 5% of doctors say contact lenses are their favorite option for this age group. If they had to choose one contact lens option for presbyopes, more than half would choose monovision. The quality of vision makes fitting easier and patient acceptance greater, an Illinois optometrist says.
However, about one-third of doctors prefer a soft multifocal lens among their contact lens options. These doctors acknowledge that monovision has a higher success rate, but they prefer the depth perception a multifocal contact lens offers.
Doctor, What Do You Prescribe
For Your Own Presbyopia?
0% Surgical correctionclear lens replacement with multifocal IOL
Source: Review of Optometry National Panel, Doctors of Optometry
Still, one in seven doctors are loyal to gas permeables among their contact lens options for presbyopes.
Now, among all the options for presbyopia correction, which would you choose for yourself? Seven in 10 doctors say that for their own eyes, they will (or do) choose progressive spectacles. About 11% will opt for monovision contact lenses.
One presbyopic doctor staunchly makes the argument for his trifocals over PALs, though he acknowledges shortcomings in cosmesis and salability of trifocals. My trifocal encompasses the full width of my 17-inch computer monitor, says Jim Bradley, O.D., of Oceanside, Calif. With a PAL, I have to keep turning my head to follow across text or columns of spreadsheet.
No doctors plan to choose surgical correction with clear lens replacement, and few (3%) will opt for monovision with LASIK.
Surgical procedures should only be considered for very special cases when no other option is viable, says optometrist Gerald Hensley, of Richburg, S.C.J.M.
Of course, with IOL implantation theres always the risk of complications, such as retinal detachment in myopes. And, its essential that the patients refractive error be corrected with the accommodative lens placed in the eye. Because if its not, youre going to have a patient whos going to require some kind of optical correction for that refractive error, in which case theres really no benefit of having an accommodative intraocular lens in the eye, Dr. Glasser says.
Future research is also likely to consider whether accommodation can be restored by injecting a silicone polymer into the capsular bag following removal of the crystalline lens The silicone polymer is designed to mimic the performance of a young, soft human lens capable of undergoing accommodative changes.
Challenging Helmholtz
But what if Helmholtzs theory of accommodation is not correct? Ophthalmologist Ronald A. Schachar says it doesnt work that way. Dr. Schachar, who has a Ph.D. in physics, argues that the physics of Helmholtzs theory dont make sense.
His own theory suggests that to accommodate, the ciliary muscle contracts and pulls on the equatorial zonules so that the lens moves toward the sclera.12,13 This equatorial pull causes the peripheral lens surface to become slightly flatter, but increases the central curvature. This central steepening provides the increase in optical power.
What other researchers have missed is that the movement of the lens toward the sclera is very small, Dr. Schachar says; the equatorial diameter of the lens undergoes less than a 5% change during accommodation.14 This movement of the lens is slight compared to relatively grosser movements of the eye. Dr. Schachar says the latter has thrown off other experiments that seek to observe the movement of the lens during accommodation to disprove his theory.
Many researchers agree that presbyopia occurs in part because the lens grows larger throughout life and thisfor one reason or anotherimpairs its ability to accommodate. But which reason is it? Helmholtzs theory was that presbyopia occurs because the lens hardens; some researchers say that hardening is partly due to the lens increased size.
Dr. Schachar also thinks the lens continues to grow but expands outward in equatorial diameter. In his model, the gap between the lens and the sclera narrows, so the tension that the ciliary muscle and zonules can exert decreases with age. Eventually, the zonules become too loose to pull on the lens. Presbyopia develops because the lens can no longer accommodate.
However, Dr. Schachar postulates that presbyopia could be reversed if a surgeon could restore an adequate distance between the ciliary muscle and the lens.15 Surgeons have attempted various methods to achieve this. The current iteration: Using four slivers of PMMA inserted in a quadrant pattern in the sclera, at a depth as far as 75% of the scleral thickness. When inserted properly, the scleral expansion bands (SEBs) should produce at least 300m of expansion between the lens and the ciliary muscle. This, Dr. Schachar says, should increase a presbyopes accommodation by 7.00D.16 Yet, results so far have been mixed.17-20
Many have challenged Dr. Schachars theory. Remember, in their work with the rhesus monkeys, Drs. Kaufman and Glasser observed that the ciliary body and the lens equator moved away from the sclera during accommodation. This supports Helmholtzs theory instead.7
For now, research into the exact causes of presbyopia appears to raise more questions than it answers. But it could lead to new frontiers in treatment, including accommodating IOLs, gene therapy, biochemical and mechanical experimentation, and perhaps laser reshaping of the lens itself.
As Dr. Koretz points out, once we look carefully at the properties of the lens, scientists may be able to figure out a way to alter lens biomechanics in a way that prevents or adjusts for presbyopia.
1. Glasser A, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision Res 1998 Jan;38(2):209-29.
2. Glasser A, Campbell MC. Biometric, optical and physical changes in the isolated human crystalline lens with age in relation to presbyopia. Vision Res 1999 June;39(11)1991-2015.
3. Croft MA, Kaufman PL, Crawford KS, et al. Accommodation dynamics in aging rhesus monkeys. Am J Physiol 1998 Dec;275(6 Pt 2):R1885-97.
4. Poyer JF, Kaufman PL, Flugel C. Age does not affect contractile responses of the isolated rhesus monkey ciliary muscle to muscarinic agonists. Curr Eye Res 1993 May;12(5):413-22.
5. Bito LZ, DeRousseau CJ, Kaufman PL, Bito JW. Age-dependent loss of accommodative amplitude in rhesus monkeys: an animal model for presbyopia. Invest Ophthalmol Vis Sci 1982 Jul;23(1):23-31.
6. Kaufman PL, Bito LZ, DeRousseau CJ. The development of presbyopia in primates. Trans Ophthalmol Soc U K 1982;102 Pt 3:323-6.
7. Glasser A, Kaufman PL. The mechanism of accommodation in primates. Ophthalmology 1999 May;106(5):863-72.
8. Koretz JF, Cook CA, Kaufman PL. Aging of the human lens: changes in lens shape upon accommodation and with accommodative loss. J Opt Soc Am A Opt Image Sci Vis 2002 Jan;19(1):144-51.
9. Koretz JF, Cook CA, Kaufman PL. Aging of the human lens: changes in lens shape at zero-diopter accommodation. J Opt Soc Am A Opt Image Sci Vis 2001 Feb;18(2):265-72.
10. Cook CA, Koretz JF, Pfahnl A, et al. Aging of the human crystalline lens and anterior segment. Vision Res 1994 Nov;34(22):2945-54.
11. Koretz JF, Cook CA, Kaufman PL. Accommodation and presbyopia in the human eye. Changes in the anterior segment and crystalline lens with focus. Invest Ophthalmol Vis Sci 1997 Mar;38(3):569-78.
12. Schachar RA. Cause and treatment of presbyopia with a method for increasing the amplitude of accommodation. Ann Ophthalmol 1992 Dec;24(12):445-7, 452.
13. Schachar RA. Zonular function: a new hypothesis with clinical implications. Ann Ophthalmol 1994 Mar-Apr;26(2):36-8.
14. Schachar RA, Tello C, Cudmore DP, et al. In vivo increase of the human lens equatorial diameter during accommodation. Am J Physiol 1996 Sep;271(3 Pt 2):R670-6.
15. Schachar RA. Pathophysiology of accommodation and presbyopia. Understanding the clinical implications. J Fla Med Assoc 1994 Apr;81(4):268-71.
16. Schachar RA. Presbyopic surgery. Int Ophthalmol Clin 2002 Fall;42(4):107-18.
17. Mathews S. Scleral expansion surgery does not restore accommodation in human presbyopia. Ophthalmology 1999 May;106(5):873-7.
18. Elander R. Scleral expansion surgery does not restore accommodation in human presbyopia. J Refract Surg 1999 Sep-Oct;15(5):604.
19. Malecaze FJ, Gazagne CS, Tarroux MC, Gorrand JM. Scleral expansion bands for presbyopia. Ophthalmology 2001 Dec;108(12):2165-71.
20. Cross W. Theory behind surgical correction of presbyopia. Ophthalmol Clin North Am 2001 Jun;14(2):315-33,viii.

