 |
On examination, visual acuity measured light perception in the right eye and 20/400 in the left. Pupil testing revealed irregularly shaped pupils that were inferiorly placed in both eyes. There was a large-angle esotropia in the right eye. On confrontation visual fields, the patient could only count fingers inferiorly. Horizontal nystagmus was present in both eyes.
The anterior segment exam revealed a dense, mature cataract in the right eye. The lens in the left eye was clear. IOP measured 8mm Hg in the right eye and 15mm Hg in the left.
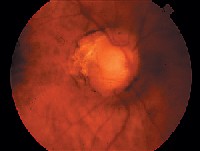
The cataract prevented any view of the right fundus. Dilated fundus exam of the left eye was significant for the changes seen in figure 1.
 |
| 1. Fundus photo of the patients left eye shows these striking features of the optic nerve and fundus. A dense cataract prevented any view of the right fundus. |
Take the Retina Quiz
1. What do the irregularly shaped, inferiorly placed pupils likely represent?
a. Surgical iridectomies.
b. Traumatic iridodialysis.
c. Iris colobomas.
d. Melt holes.
2. What additional testing would be most beneficial?
a. Computed tomography.
b. Visual field.
c. Ultrasound.
d. Electroretinogram.
3. What is the correct diagnosis?
a. Iridocorneal endothelial syndrome.
b. Regressed retinoblastoma.
c. Combined iris, chorioretinal and optic nerve coloboma.
d. Morning glory syndrome.
4. An additional finding that is often present with this condition was present on the entrance exam but not disclosed in the history. What else does this patient have?
a. Macular hole.
b. Microphthalmia.
c. Choroidal neovascular membrane.
d. Subluxation of the lenses.
5. What is the most significant complication that can occur in the patients left eye?
a. Glaucoma.
b. Perforation.
c. Retinal detachment.
d. Recurrence of the tumor.
For answers, see bottom of page.
The irregular-shaped pupils that were inferiorly placed represent iris colobomas. Also, the striking changes in the fundus of the left eye represent chorioretinal colobomas and a coloboma of the optic nerve. Ciliary body coloboma may have been present, but we were not able to see this.
Colobomas result from an abnormal closure of the developing optic vesicles at the seventh week of embryonic development.1 If the anterior end of the embryonic fissure fails to close, colobomas can develop in the iris, ciliary body and choroid. If the posterior end fails to close, a coloboma of the optic disc will result.1
The colobomas mentioned here often occur in combination, as in our patient, when there is complete failure of the fissure to close.
Microphthalmia is common when iris, choroidal and optic nerve colobomas are present.2 This information was not disclosed in the history, but indeed was present in our patient. Her right eye was much more microphthalmic than the left. The large-angle esotropia in the patients right eye was due to sensory deprivation.
Optic nerve coloboma typically appears as a large, glistening, white bowl-shaped excavation that occupies the area of the optic nerve. The excavation extends inferiorly when the choroid is involved and can extend anteriorly to the ciliary body.
The superior retina and choroid typically are not affected. However, there is a significant risk of rhegmatogenous retinal detachment due to the thinned retina overlying the colobomatous defect.1
The details of our patients optic nerve are almost impossible to distinguish. There is a large excavation where the nerve should be, an abnormal blood vessel pattern coming out of and around the optic nerve, and several smaller pockets of excavated colobomatous choroid or lacunae around the nerve.
 |
 |
| 2, 3. Morning glory syndrome (left) and forme fruste of morning glory syndrome are seen here in other patients. Morning glory syndrome, which can be confused with our patients condition, presents with excavation of the optic nerve, but this excavation takes on more of a funnel shape, incorporates the optic nerve and resembles a morning glory flower. Courtesy: Joseph W. Sowka, O.D., Andrew S. Gurwood, O.D., Alan G. Kabat, O.D. |
Sometimes it can be difficult to distinguish between this patients condition and morning glory syndrome. Morning glory also presents with excavation of the optic nerve, but this excavation takes on more of a funnel shape, incorporates the optic nerve and resembles a morning glory flower.2
The optic nerve in patients who have morning glory syndrome typically is very large and has an orange or pink coloration. The optic nerve also has fibroglial tissue in the center of the nerve. Finally, pigmentary changes surround the optic nerve.
Our patient did not have any orange or pink coloration, but a hint of fibroglial tissue was present. The excavation with optic nerve coloboma usually involves only the optic nerve, unless there is a combined coloboma of the choroid, as our patient had.
Also, morning glory is largely unilateral, while optic nerve colobomas can be unilateral or bilateral with equal frequency.2 Our patient has bilateral colobomas.
We could not determine the extent of involvement in the right eye due to the dense cataract. However, we can assume that changes similar to those in the left eye exist in the right eye, as this patient has the iris coloboma and much more microphthalmia. These things could indicate more severe involvement of the coloboma.
We advised the patient to have an ultrasound in the right eye, but she failed to return for follow-up. We also discussed cataract surgery for the right eye, but her family believed that there would be minimal benefit.
Finally, we recommended that the patient wear protective eyewear and undergo a low vision exam so that she could optimize the vision potential she had in the left eye.
1. Barishak YB, Spierer A. Embryology of the posterior segment and developmental disorders. In: Pediatric Retina. Hartnett ME, Trese M, Capone A Jr., et al. Philadelphia: Lippincott Williams and Wilkins, 2004:3-12.
2. Brodsky M. Congenital optic disc anomalies. In: Taylor D, Hoyt C. Pediatric Ophthalmology and Strabismus. 3rd ed. New York: Elsevier Saunders, 2005:625-45.
Answers: 1) c; 2) c; 3) c; 4) b; 5) c.

