 |
A 53-year-old Hispanic female presented on an emergent basis with complaints of blurred vision and difficulty focusing in her right eye for the past two days. His medical history was significant for a stroke involving the left hemisphere, also four years prior, as well as Type 2 diabetes, which was diagnosed nine years ago and is being treated with metformin and insulin injections.
She reported blurry vision when she woke up, as well as seeing floaters and colored lights in the same eye. She denied any viral or flu-like illnesses, and her past ocular history was significant for trauma in the left eye as a child that resulted in a corneal scar. Because of this, she has always had a significant difference in refractive error between her two eyes but usually wears contact lenses, which helps. Her medical history is unremarkable.
Upon exam, best-corrected visual acuity was 20/50 OD and 20/25 OS. Ocular motility and cover testing were normal. Confrontation visual fields were full to careful finger counting OU. Pupils were equally round and reactive to light; there was no afferent pupillary defect. The anterior segment of the right eye was unremarkable, and the left eye was significant for a geographic corneal scar that involved the axis.
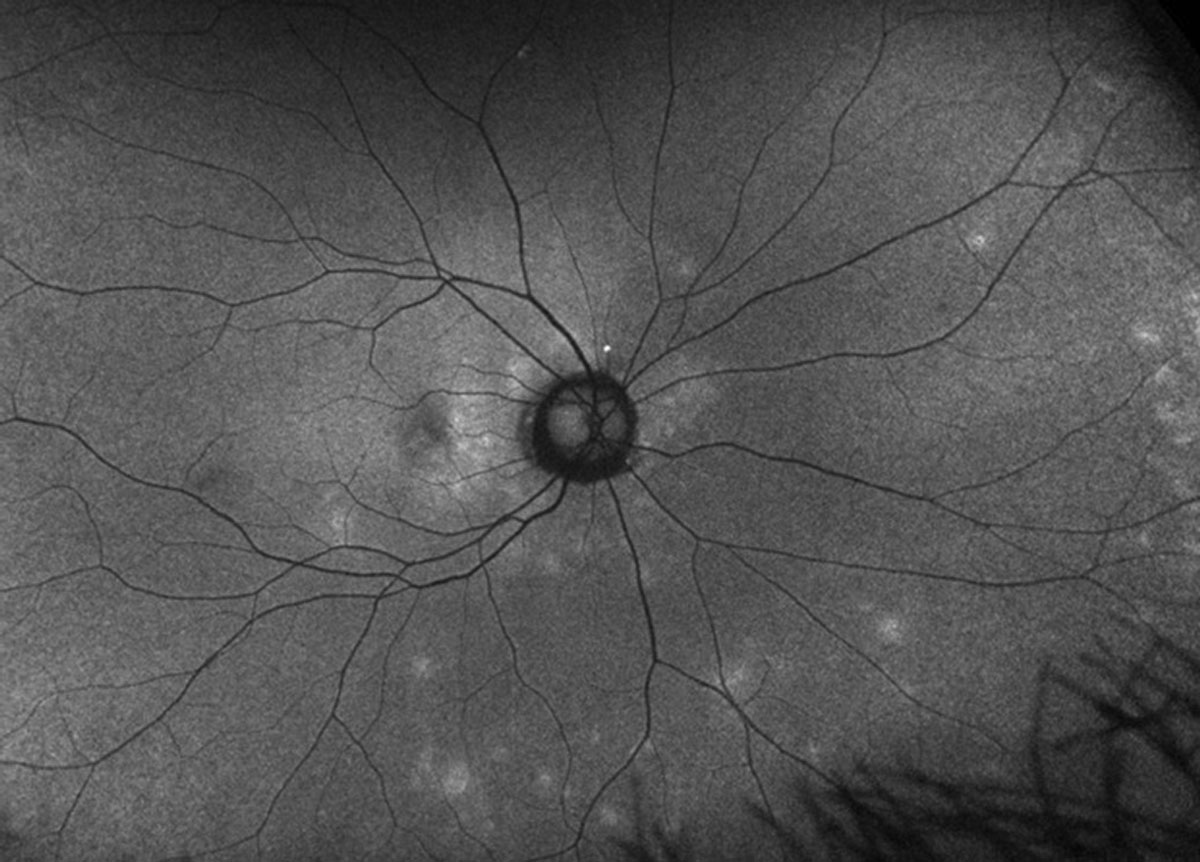
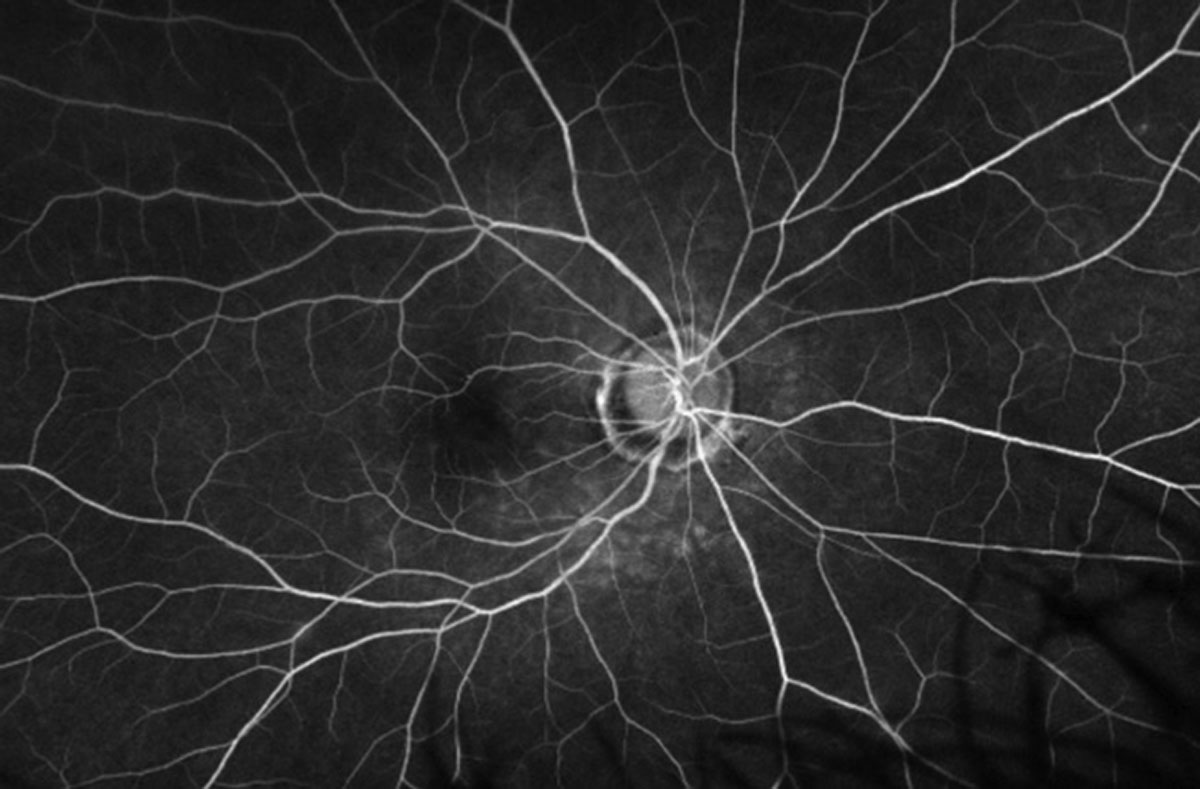
Dilated fundus exam of the right eye showed a clear vitreous and normal-appearing optic nerves with good rim coloration and perfusion. The rest of the right eye findings appeared normal; however, on closer inspection there were peculiar changes (Figure 1). The left eye was completely normal. A fluorescein angiogram, OCT (Figure 2) and fundus autofluorescence (FAF) were performed (Figure 3). An image from late in the angiogram is available for review (Figure 4).
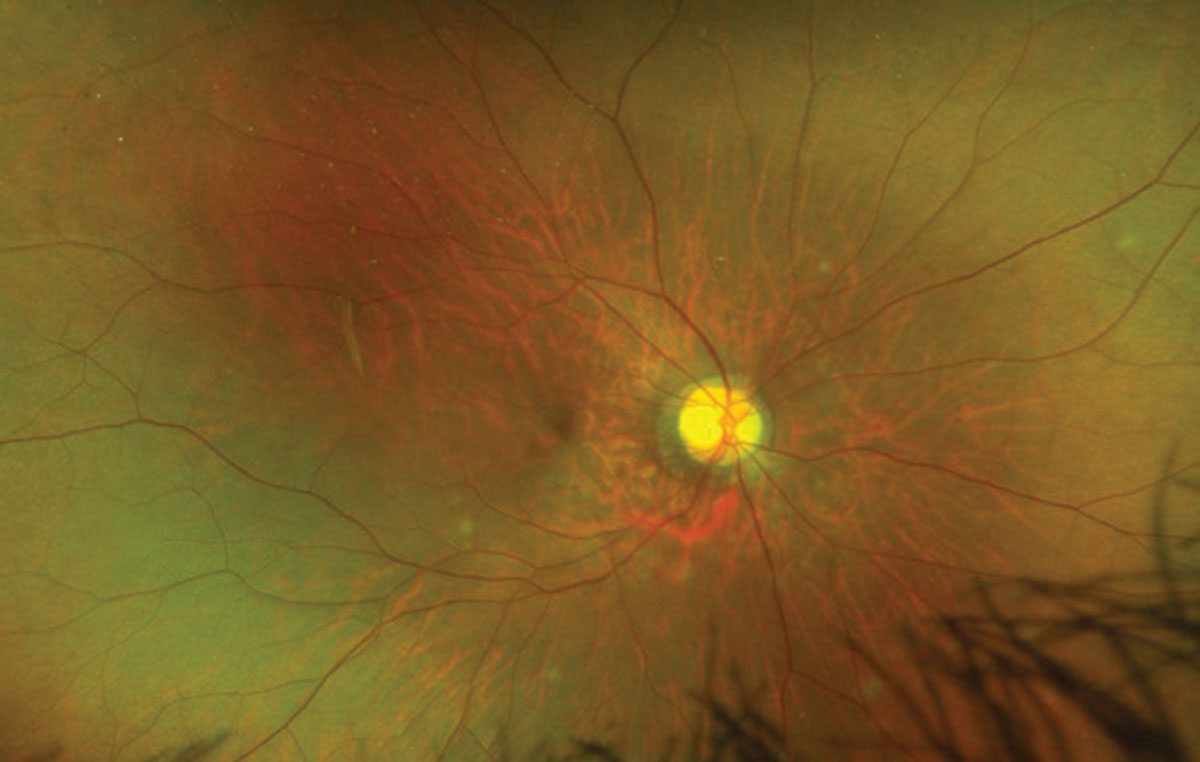 |
Fig. 1. Look carefully around the optic nerve and inferior arcade in this patient’s right eye. Click image to enlarge. |
Take the Retina Quiz
1. What does our patient have?
a. Acute macular neuroretinitis (AMN).
b. Multiple evanescent white dot syndrome (MEWDS).
c. Diffuse unilateral subacute neuroretinitis (DUSN).
d. Birdshot retinochoroiditis.
2. What is the most likely etiology?
a. Autoimmune.
b. Viral.
c. Infectious.
d. Inflammatory.
3. How should she be managed?
a. Observation.
b. Oral presnisone 80mg.
c. Anthelmintic drugs (thiabendazole).
d. Oral antiviral agent (Valtrex).
4. Which is the likely clinical course?
a. Progressive with total loss of vision.
b. Chronic and recurrent with loss of central vision.
c. Episodic recurrences with generally good vision.
d. Self-limited with good recovery of central vision.
For answers, see below.
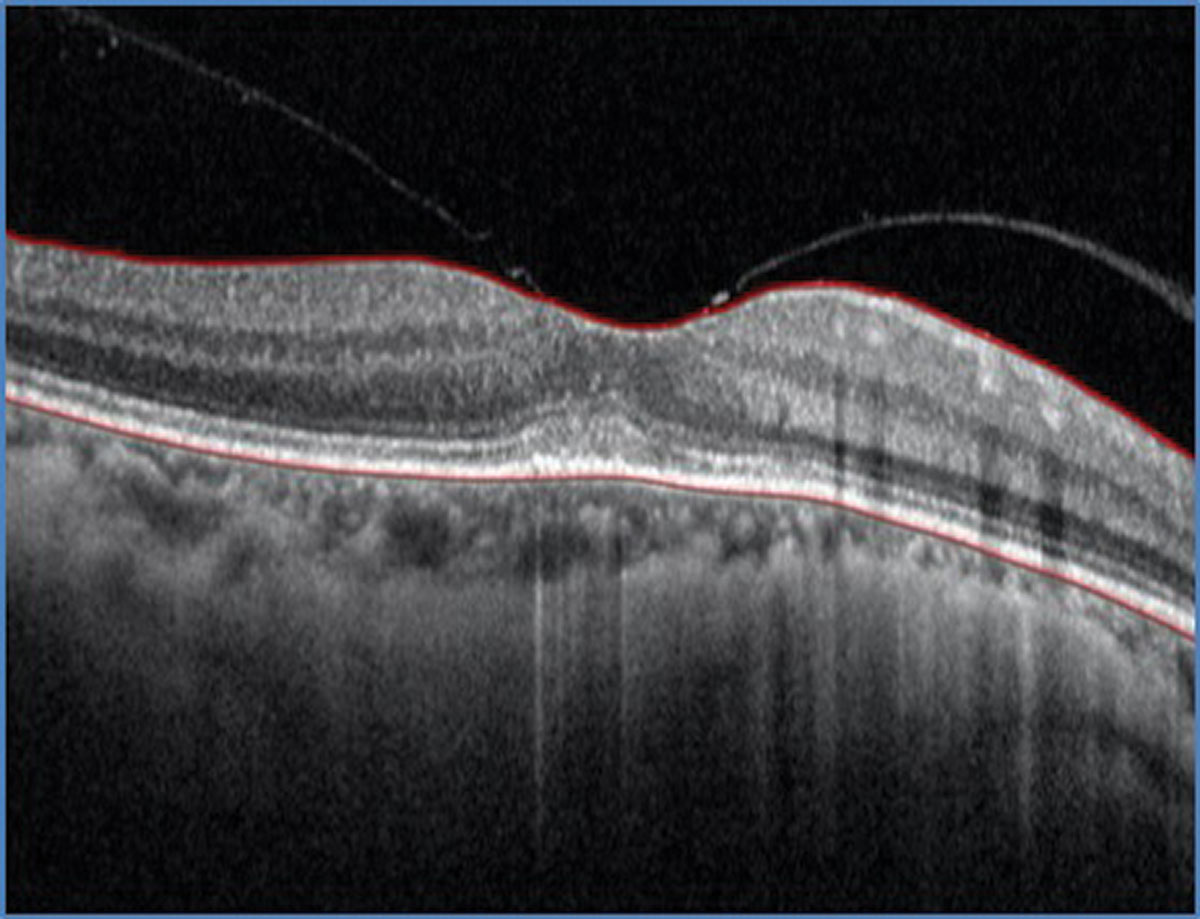 |
| Fig. 2. SD-OCT through the macula of the left eye. What does it show? Click image to enlarge. |
Discussion
There are multiple small gray-white “spots” scattered throughout the posterior pole in the right eye of our patient. They are subtle, but can more easily be seen along the inferior arcade below the macula and also extending to the nasal side of the optic nerve. These spots are more easily observed on the FAF, where numerous hyperfluorescent lesions can be seen scattered throughout the posterior pole; many more than what we were able to see on the clinical exam and appear to be concentrated around the optic nerve and extend into the macula. The fluorescein angiogram shows late staining of the lesions and confirms that these are located in the outer retinal layers.1
So, what’s going on with our patient? She probably has a post-viral retinal syndrome—likely multiple evanescent white dot syndrome, or MEWDS as it is commonly known. MEWDS was originally described in 1983 as an acute, unilateral, multifocal retinopathy that affects young adults—most commonly females in 75% of reported cases.1 Approximately one-third of patients report having a flu-like or viral illness before developing vision loss.1-3 Our patient denied having any such symptoms, but she did report receiving the COVID-19 vaccine about six weeks earlier. When asked about travel history, she reported having gone to Colorado a few weeks prior.
The age of presentation of MEWDS ranges from 14 to 57 years old.1,2 Patients most commonly complain of blurred vision in addition to photopsia or flashing lights, and clinical findings include small, multifocal gray-white spots that are mostly concentrated in the paramacular area. The macula will usually have a granular appearance with tiny yellow or orange dots in the center of the fovea that may disrupt the IS/OS junction.1-3 Though we did not appreciate these changes in the macula on clinical exam, she does have some mild disruption in the outer retinal layers on the OCT. Most patients with MEWDS will have a mild vitritis; this was not present in our patient. In addition to the blurred vision and photopsia, patients may also have an enlarged blind spot on visual field testing which has emerged as part of the spectrum of MEWDS.
 |
|
Fig. 3. FAF image of the right eye. How is it different than the clinical photo? Click image to enlarge. |
Imaging studies such as fluorescein angiography (FA), FAF and indocyanine green (ICG) may be helpful in establishing a MEWDS diagnosis. On fluorescein angiography the gray-white patches will hyperfluorescence in a “wreath-like” pattern, which was seen in our patient. FAF also shows hyperfluorescence, but interestingly ICG will show hypofluorescence spots. Both imaging modalities will reveal spots in greater numbers than what is seen on the clinical exam—we were able to clearly see this on the FAF. ICG was not performed, as we felt we had enough information to establish a diagnosis without needing to do additional testing.
The natural history of MEWDS is a complete recovery of the vision over a period of several weeks; therefore, no treatment is recommended. The white patches and granular appearance in the macula will slowly fade away over time and become less apparent. This can make the diagnosis even more challenging, depending on when the patient is seen.
The etiology of MEWDS remains a mystery. It is thought to be related to a viral illness, but so far none of the more common viral etiologies such as herpes zoster, herpes simplex, measles or mumps have been identified as a source. MEWDS is a disease of the photoreceptors and is almost completely reversible. It can be considered a “common cold” of the retina.3
Our patient presented with symptoms that began only two days earlier. She was seen one month later and her visual acuity had improved back to 20/20 and white spots were nearly gone.
 |
|
Fig. 4. Late frame of the FA of the right eye. Click image to enlarge. |
Retina Quiz Answers
1) b; 2) b; 3) a; 4) d.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
| 1. Aaberg TM, Campo RV, Joffe L. Recurrences and bilaterality in the multiple evanescent white-dot syndrome. Am J Ophthalmol. 1985; 100:29–37. 2. Jampol LM, Sieving PA, Pugh D, et al. Multiple evanescent white dot syndrome. I. clinical findings. Arch Ophthalmol. 1984; 102:671–4. 3. Tavallali A, Yannuzzi LA. MEWDS, A common cold of the retina. J Ophthalmic Vis Res. 2017; 12(2):132‐4. |

