 |
The cornea is rather dumb. At least that’s what Daniel Durrie, MD, told me during my cornea fellowship in the mid ’90s. These words of wisdom from one of the top cornea and refractive surgeons have stuck with me to this day.
Unlike most other tissues, the cornea has no blood vessels or lymphatics and thus has limited potential responses to disease or injury—only five, in fact: thin, infiltrate, break down/abrade, deposit and swell (although I’ve added two subcategories here). Once you understand these, you can recognize and effectively manage every corneal presentation. Here’s the life of a compromised cornea and its limited responses:
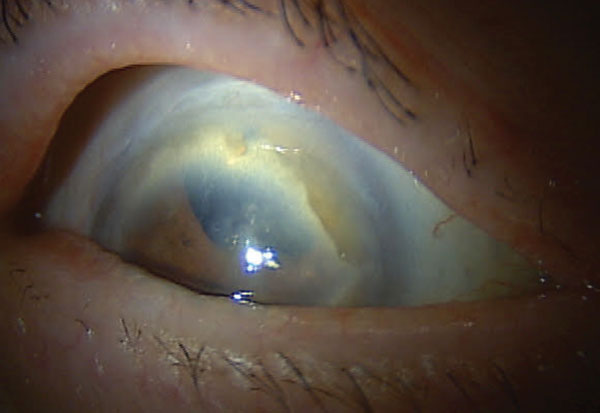 |
| Fig. 1. Like many with Terrien’s marginal degeneration, this patient has corneal thinning. |
1. Thin
This includes keratoconus, as progression not only affects Ks and, eventually, refraction but also peripheral corneal thickness. To determine early keratoconus or pellucid marginal degeneration, look at the peripheral cornea at 5, 6 and 7 o’clock. Normally, the cornea thickens by 20µm to 50µm as you move to the periphery. A peripheral cornea that isn’t at least 20µm thicker than the central cornea is suspect.
New surgical advances such as corneal crosslinking for early cases of keratotconus and deep anterior lamellar keratoplasty (DALK) are showing great success in advanced ectasia cases. Find surgeons with experience with DALK so you can best manage your patients with keratoconus. Other conditions that cause thinning include peripheral degenerations such as Terrien’s or furrow degeneration (Figure 1).
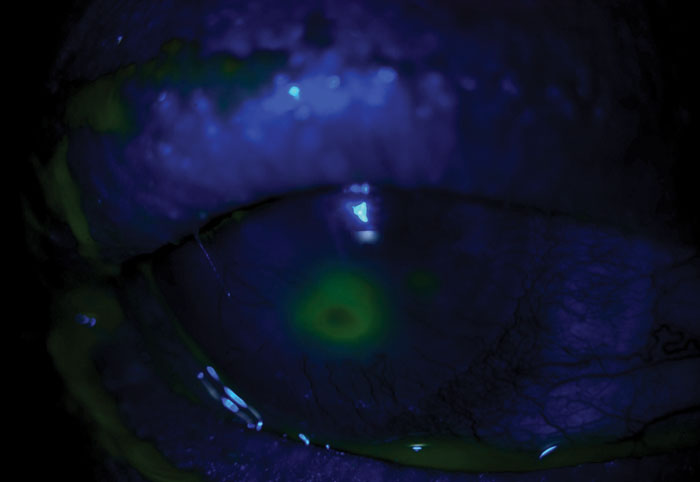 |
| Fig. 2. Corneal ulceration requires urgent management to avoid long-term visual consequences. |
• Subcategory—Ulcerate. Although this also fits in the category of thinning, it’s on its own here because of the need for urgent management (Figure 2). Ulceration can be infectious or non-infectious. Corneal infections range from bacterial keratitis and herpes dendritic epithelial keratitis to the rarer fungal and parasitic forms such as Acanthamoeba.
It can also be non-infectious, such as those related to a neurotrophic cornea or inflammatory in cases of rheumatoid corneal melts and Mooren’s ulcers.
2. Infiltrate
Because the vasculature is outside the cornea, white blood cells can’t directly get to the tissue; however, they can infiltrate and form within the cornea. Pathogens can also penetrate or infiltrate the cornea if given an opportunity. The presentation of infiltration can vary from extreme, as in the case of an advanced microbial keratitis, to lesser degrees as seen in epidemic keratoconjunctivitis, peripheral marginal keratitis or Staphylococcal hypersensitivity.
Suppressing white blood cells to prevent corneal scarring may involve aggressive infection control when the underlying cause is infectious, or steroids when it is inflammatory (Figure 3). I include vascularization in this category as well, considering it is the body’s response to corneal infiltration.
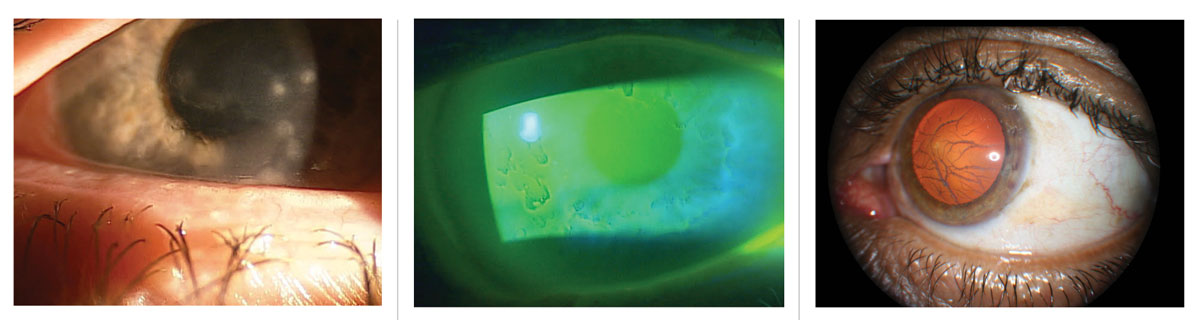 |
| Figs. 3-5. Preventing corneal scarring is key when treating corneal infiltrates (left). Epithelialbasement dystrophy can cause recurrent corneal erosion (middle). Lattice corneal dystrophy is characterized by amyloid deposition (right). Click image to enlarge. |
3. Break Down/Abrade
The epithelium serves to protect the delicate nerves and structures of the cornea but can be abraded by trauma or other conditions such as recurrent corneal erosion (RCE) (Figure 4). My protocol for managing recurrent corneal erosion, especially recalcitrant forms, has changed over the years with the advent of amniotic membrane, which now plays an early and important role.
 |
| Fig. 6. Patients with Fuchs’ dystrophy often have visual symptoms, such as halos, due to corneal edema. Click image to enlarge. |
4. Deposit
Various compounds can accumulate in the cornea and disrupt its function (Figure 5). The deposits can be due to genetic causes such as corneal dystrophies, epithelial basement dystrophy with the deposition of redundant basement membrane, drugs (e.g., amiodarone) and even compounds such as copper (Wilson’s disease) and cholesterol (arcus senilis, lipid keratopathy and Snyder’s crystalline dystrophy).
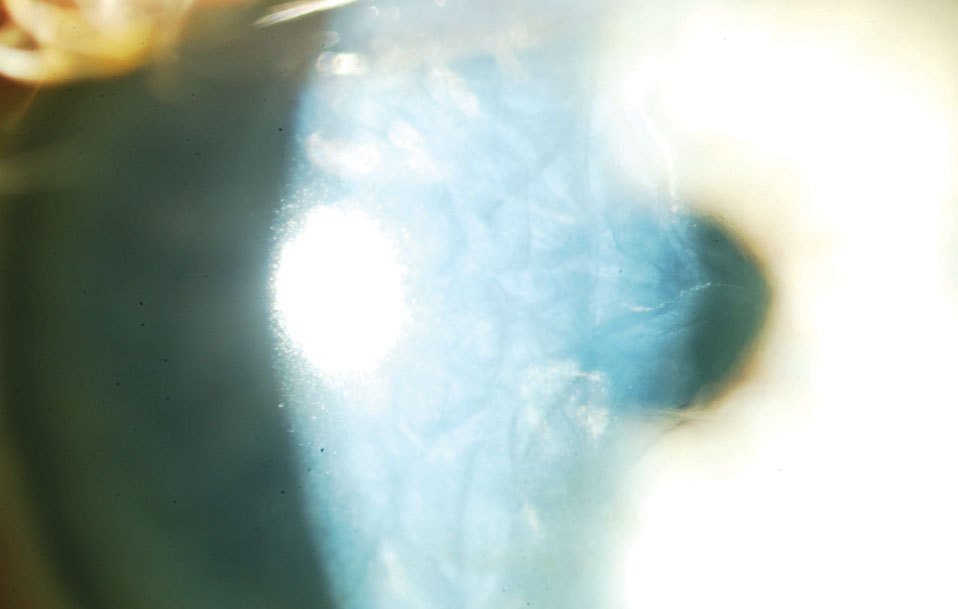
• Subcategory—Scar. This phenomenon is arguably a deposition of scar tissue or calcium, as in band keratopathy, thus limiting the cornea’s vocabulary to only five functions. Scarring has its own subcategory here simply because it is the end stage of disease for the cornea.
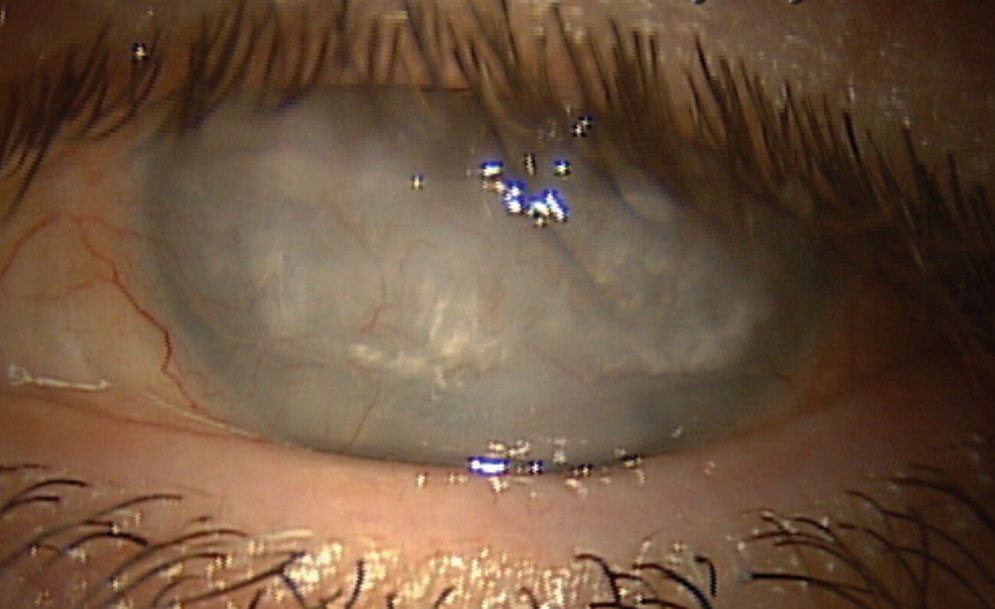 |
Fig. 7. This patient who experienced a central retinal artery occlusion later developed band keratopathy and corneal scarring. Click image to enlarge. |
5. Swell
The purpose of the endothelium is primarily to prevent edema within the cornea. Our endothelial cells continuously pump fluid out of the cornea, especially in the morning to overcome the natural overnight corneal swelling. When this delicate balance is affected, as in cases of Fuchs’ dystrophy, patients notice blurring, particularly in the morning, and night vision problems such as halos (Figure 6). Specular microscopy, once thought to be a tool reserved for cornea specialists, is making its way into primary eye care offices as the only way to monitor endothelial health and make a proper and timely referral to a cornea specialist.
This approach is a significantly different way to look at the cornea, but one I often use when seeing patients referred for unknown corneal presentations. Sometimes, categorizing the cornea’s response can make a huge difference in both the final diagnosis and the optimal treatment strategy. The cornea’s limited vocabulary helps all of us who manage corneal disease regularly; there isn’t much else this unique and vital tissue can do, and knowing the five essential presentations is key.

