By CHARLES SLONIM, M.D.
Tampa, Fla.
There is a misguided yet widespread belief that allergy sufferers are better off wearing glasses than contact lenses. Granted, there is logic behind this belief. However, there are ways of dealing both with patients" allergies and their burning desire to continue wearing contact lenses throughout their worst allergic seasons.
Allergy sufferers who wear contact lenses are likely to have a di fficult time with ocular itching, tearing, dryness and redness during periods of allergic conjunctivitis, be it giant papillary conjunctivitis or due to seasonal, atopic or perennial allergies. Many of these patients are on systemic medications--antihistamines or decongestants--that are known to cause ocular surface drying and are often associated with difficulty achieving comfortable lens wear.
 |
|
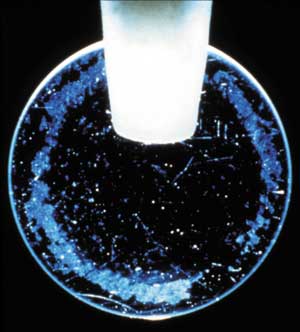
Protein buildup can cause a type of allergic inflammatory response similar to what"s provoked by environmental allergens such as animal dander. |
Specific to Lens Wear
My experience in more than 20 years of practice has been that many allergy sufferers who wear contact lenses complain of itching and discomfort associated with their lenses during allergy season. These symptoms may be related to the hydrogel material absorbing the aqueous tear film to support the water-based polymers, or they may stem from the changing nature of proteins elaborated in the tears during periods of acute allergy. An allergic inflammatory response brings an upregulation, or a "turning on," of the epithelial surface receptors that bind eosinophils and other neutrophils. Upregulating these receptors may prime allergy patients to be more sensitive to symptoms of discomfort, especially when wearing a contact lens.
It"s well established that contact lens wearers have reduced tear flow. This diminishes the eye"s ability to dilute and remove environmental allergens from the ocular surface. A dryer ocular surface is more susceptible to tissue damage from the allergic inflammatory response.
It"s generally accepted that even with the best-fitting soft contact lens, numerous microscopic epithelial defects will occur on the ocular surface. Some of these will be visible under the slit lamp, but many will not. These findings are not much different from what we find in a patient with a very mild dry eye syndrome. Corneal epithelial defects have less surface protection from allergen (protein) binding.
Patients with allergies may be more sensitive to further surface insults such as contact lens wear, dry eye or LASIK. Patients with chronic mild inflammation tend to have a more rapid turnover of epithelial cells from the surface. Contact lens wearers may therefore have a greater risk of developing more frequent and more severe allergic reactions when encountering certain allergens.
The Rationale for Daily Disposables
Even under ideal wearing conditions, soft lenses inevitably contain surface proteins. However, it is well established in the literature that as lenses age and are exposed to the environment, more protein binding occurs and the lenses lose their natural molecular shape, becoming "denatured." The body may then react as if the protein build-up were a foreign substance, provoking a range of allergic symptoms and signs, from mild discomfort to giant papillary conjunctivitis. This can create a type of allergic inflammatory response similar to that of the environmental allergen to which the patient is known to be allergic (pollens and animal dander, for example).
It is my belief that by replacing contact lenses each day, wearers can limit the buildup of this "bad" protein as well as the amount of time this substance is in contact with the eye and eyelids. By discarding their lenses daily, allergy sufferers discard the surface proteins with which they may have come in contact during their normal daily activities. In addition, eliminating the chemicals in lens care systems adds an extra benefit for patients who may also be more sensitive to chemical stimuli during periods of allergic response.
The Daily Disposable Advantage
Fortunately, advances in disposable contact lenses mean new hope for the estimated 50 million Americans with allergies.
For instance, the Food and Drug Administration recently recognized that Acuvue contact lenses worn on a daily disposable basis may provide improved comfort for patients with mild allergic discomfort and ocular itching compared with contact lenses replaced less often than every two weeks. The new claim is based on a recent clinical study showing that two out of three allergy sufferers preferred the comfort of one-day Acuvue lenses to what they experienced with a new pair of their habitual lenses. The investigators in the study also noted a significant improvement in the severity of ocular signs associated with allergies--bulbar and palpebral redness, corneal staining and lid roughness--in those wearing one-day Acuvue lenses compared with the pre-study baseline levels.
This is good news, especially for those who suffer from hayfever (allergic rhinitis) but who don"t want to resort to wearing their spectacles during the high-pollen-count days of spring. And that"s not even counting the many contact lens wearers who may have perennial allergies; in the one-day Acuvue study, 80% of the subjects reported that they suffered from allergic symptoms year-round.
A significant proportion of our contact lens wearers will surely appreciate whatever measures you can take to ease their allergic symptoms and provide for trouble-free lens wear. For many, relief is in sight, thanks to daily disposables.
Dr. Slonim is clinical professor of ophthalmology at the University of South Florida College of Medicine in Tampa, Florida.

