 Iritis, or iridocyclitis, is a common form of anterior
uveitis that is frequently observed in clinical practice. It can lead to
long-term debilitation, synechiae and secondary glaucoma.1
Here, we examine research on the latest treatments for
iritis and provide six clinical pearls to help you manage this prevalent ocular
pathology.
Iritis, or iridocyclitis, is a common form of anterior
uveitis that is frequently observed in clinical practice. It can lead to
long-term debilitation, synechiae and secondary glaucoma.1
Here, we examine research on the latest treatments for
iritis and provide six clinical pearls to help you manage this prevalent ocular
pathology.
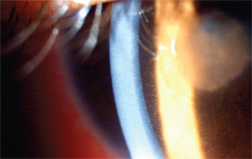 |
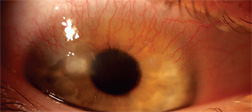
| Iritis, as seen in this patient, is a common form of anterior uveitis that can cause long-term debilitation, synechiae and secondary glaucoma, if left untreated. |
The goals of iritis treatment are to minimize permanent structural alterations of aqueous outflow and prevent optic nerve damage. An aggressive regimen is required, which may include Pred Forte (prednisolone acetate 1%, Allergan) q1h as well as nighttime application of a topical corticosteroid, such as Maxitrol (neomycin/polymyxin B/dexamethasone, Alcon) or Tobradex (tobramycin/dexamethasone, Alcon).
More recently, Durezol (difluprednate 0.05%, Sirion Therapeutics), a synthetic difluorinated prednisolone derivative, has proven very effective for the treatment of post-cataract surgery iritis and pain.2,3 Durezol received FDA-approval for dermatological application in June 2008. The drug derives its potency from fluorination at the C6 and C9 position.4 Durezol is also an oil-in-water emulsion (castor oil), which allows poorly soluble drugs, such as prednisolone, to dissolve in the oil phase, eliminating the need to shake the bottle.5 Finally, Durezol contains no benzalkonium chloride and demonstrates higher bioavailability than comparable ophthalmic suspensions.6
 |
| To produce a good visual outcome, treat iritis agressively
with corticosteroids.
|
1. Differentiate iritis from keratouveitis. First, you must differentiate iritis from keratouveitis. Look for the presence of corneal infiltrates and/or epithelial defects. This is critically important, because an iritis that doesn’t involve the cornea is typically managed with corticosteroids and cycloplegic agents. On the other hand, the use of corticosteroids for a keratouveitis is contraindicated in most cases due to the likelihood of microbial keratitis development or unwanted immunosuppression.7
2. Check IOP. Next, measure the patient’s intraocular pressure. Research suggests that a typical iritis might actually reduce IOP.8 (In some cases, however, concurrent iritis and trabeculitis can actually cause an increase in IOP.9) Secondary glaucoma can be caused by several acute or chronic mechanisms, and is often associated with open or closed angles, synechiae formation, pupillary block, neovascularization and even anterior rotation of the lens-iris diaphragm.5,10 In general, elevated IOP associated with a uveitis can be the result of active inflammation, corticosteroid therapy, insufficient glaucoma therapy, or permanent changes in the ocular structures that alter aqueous humor dynamics.11 In the case of elevated IOP secondary to uveitis, treatment with potent corticosteroids often lowers the pressure.12 Be aware, however, that steroid responders may experience an elevation in IOP over time.5 For this reason, you should monitor patients on corticosteroid therapy closely, prescribe concurrent pressure lowering agents, and consider an ester-based steroid, such as Lotemax (loteprednol 0.5%, Bausch & Lomb) if long-term management is required.13-15
3. Rule out endophthalmitis. Significant iritis following cataract surgery, with a correspondent decrease in vision and pain, is a hallmark sign of potential endophthalmitis. While many clinicians look for endophthalmitis to occur immediately after cataract surgery, the mean time of onset is actually 9.2 days post-op.16
4. Look for a systemic cause. Gauge the severity of the iritis and order appropriate lab tests or refer to an internist to help discover a potential systemic cause. Severe iritis is likely to be secondary to a systemic condition, such as arthritis, lupus, sarcoidosis, Reiter’s syndrome, Crohn’s disease, Behçet’s disease and ankylosing spondylitis.17 Indicators of uveitis secondary to one of these systemic conditions include repeated bouts of iritis, bilateral presentation, keratic precipitates, peripheral anterior synechiae (PAS) and granulomatous uveitis.18 One study suggested that more than 18% of patients with a uveitis associated with a systemic condition developed secondary glaucoma, indicating that these patients need to be monitored regularly.19
5. Treat aggressively. Once you have ruled out a keratouveitis, begin aggressive dosing of corticosteroids at least q1h to q2h. (However, q.i.d. dosing is recommended if using Durezol.2,3) You can always taper the dose once a significant impact has been made on the iritis. Remember, passively-treated, low-grade iritis is the most common cause of secondary glaucoma in uveitis patients.20
6. Reestablish the blood-aqueous barrier. During the course of uveitis, the blood-aqueous barrier is broken down due to an influx of protein and inflammatory cells.5,21,22 So, in order to reestablish this barrier, you must continue to taper corticosteroid therapy beyond elimination of anterior chamber cell and flare.
New, potent steroids, such as Durezol, and safer, long-term medications, such as Lotemax, will help you treat iritis with greater efficacy. Additionally, if you differentiate keratouveitis, check IOP, rule out endophthalmitis, look for a systemic cause, treat aggressively and reestablish the blood-aqueous barrier, you will be in an excellent position to manage iritis more effectively in clinical practice.
Neither Dr. Karpecki nor Dr. Shechtman have any direct financial interest in the products mentioned.
1. Thean JH, Hall AJ, Stawell RJ. Uveitis in herpes zoster ophthalmicus. Clin Exp Ophthalmol. 2001 Dec;29(6):406-10.
2. Jamal KN, Callanan DG. The role of difluprednate ophthalmic emulsion in clinical practice. Clin Ophthalmol. 2009;3:381-90.
3. Korenfeld MS, Silverstein SM, Cooke DL, et al. Difluprednate ophthalmic emulsion 0.05% for postoperative inflammation and pain. J Cataract Refract Surg. 2009 Jan;35(1):26-34.
4. Bikowski J, Pillai R, Shroot B. The position, not the presence, of the halogen in corticosteroids influences potency and side effects. J Drugs Dermatol. 2006;5(2):125-30.
5. Yamaguchi M, Yasueda S, Isowaki A, et al. Formulation of an ophthalmic lipid emulsion containing an anti-inflammatory steroidal drug, difluprednate. Int J Pharm. 2005 Sep 14;301 (1-2):121-8.
6. Inoue J. Preclinical pharmocokinetics of difluprednate ophthalmic emulsion. Poster B741, program 2651. Presented at the Association for Research in Vision and Ophthalmology’s Annual Meeting. Ft. Lauderdale, Fla., May 2007.
7. Aasuri MK, Venkata N, Kumar VM. Differntial diagnosis of microbial keratitis and contact lens-induced peripheral ulcer. Eye Contact Lens. 2003 Jan;29(1 Suppl):S60-2.
8. Schubert HD, Federman JL. The role of inflammation in CW Nd:YAG contact transscleral photocoagulation and cryopexy. Invest Ophthalmol Vis Sci. 1989 Mar;30(3):543-9.
9. Besada E, Frauens BJ. Unilateral granulomatous post-streptococcal uveitis with elevated tension. Optom Vis Sci. 2008 Nov;85(11):E1110-5.
10. Pleyer U, Ruokonen P, Heinz C, et al. Intraocular pressure related to uveitis. Ophthalmologe. 2008 May;105(5):431-7.
11. Mermoud A. Physiopathology of uveitic glaucoma. Klin Monatsbl Augenheilkd. 1997 May;210(5):269-73.
12. Panek WC, Holland GN, Lee DA, et al. Glaucoma in patients with uveitis. Br J Ophthalmol. 1990 Apr;74(4):223-7.
13. Pavesio CE, Decory HH. Treatment of ocular inflammatory conditions with loteprednol etabonate. Br J Ophthalmol. 2008 Apr;92(4):455-9.

