  |
Patients with intractable corneal disease no longer have to submit to penetrating keratoplasty and tolerate its many compromises. Lamellar procedures that remove only diseased tissue have reshaped the field. Descemet’s membrane endothelial keratoplasty, or DMEK, is the latest incarnation in the evolution of posterior lamellar keratoplasties in the treatment of endothelial dysfunction. Because its development can best be understood relative to its predecessors, a brief review of these forbearers is instructive.
Evolution of DMEK
Posterior lamellar keratoplasty (PLK) and deep lamellar endothelial keratoplasty (DLEK, essentially PLK adapted for use in the United States) were the earliest posterior keratoplasties. Though these two procedures represented the first successful sutureless corneal transplants, they were too technically difficult to gain widespread adoption. Descemet’s stripping endothelial keratoplasty (DSEK) eliminated the most difficult step of the PLK and DLEK procedures—dissection of the host posterior stroma—thereby bridging the gap between postoperative success and intraoperative simplicity. With this step out of the way, DSEK was widely embraced by corneal specialists.
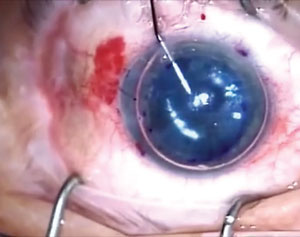
 | |
| A DMEK graft is stained with trypan blue to allow intraoperative visualization. |
DSEK uses donor tissue that’s comprised of Descemet’s membrane, endothelium and a small amount of posterior stroma. The latter, while not necessary for the function of the graft, helps surgeons handle the graft intraoperatively and insulates the endothelium to some degree from surgical trauma. However, while 20/20 and 20/25 outcomes were not unheard of with DSEK, and subsequently Descemet’s stripping automated endothelial keratoplasty (DSAEK), it was much more common for best-corrected outcomes to hover around 20/40. Investigators believed this limitation on vision was due to optical interference at the donor/host stromal interface. To get around this limitation, DMEK—in which the graft has no posterior stroma—was developed.1
Benefits of DMEK
The new procedure has delivered better BSVA outcomes than its predecessors, with 20/25 outcomes the reported average.2 Further, while DSEK and DSAEK generate an average hyperopic shift of 1D to 2D, the very thin DMEK graft does not. An interesting and unexpected benefit of DMEK is the significantly lower rate of immunologic rejection compared with DSEK and DSAEK.3 An early prospective study on DMEK reported just a 1% rate of rejection compared to 12% with DSAEK—a surprising finding given the two transplants are close to identical from an immunologic standpoint.2 DSAEK only carries additional posterior keratocytes, which have very little potential to generate rejection on their own.
DMEK Downfalls
These improvements come with a cost, however. Due to “elastic” behavior of the thin DMEK graft, it rolls into a scroll once removed from donor stroma. Unrolling the graft in the anterior chamber can be difficult, as directly handling the graft can lead to failure of the transplanted endothelium. Surgeons must therefore rely on indirect manipulation to unroll the transplant (e.g., via use of percussive waves and irrigation).
 | |
| Once the graft is positioned, a mixture of air and SF6 is put into the anterior chamber to help hold the graft in place. |
Further, these grafts have a tendency to dislocate from the host stroma early in the postoperative course at higher rates than DSEK and DSAEK. To get around this complication, larger air fills are typically used with DMEK; in our facility we use a 90% air fill with sulfur hexafluoride (SF6) high-density gas (with an inferior peripheral iridotomy to avoid pupillary block).
The Comanaging Optometrist’s Role
Preservation of the transplant and visual rehabilitation are integral to managing these patients. Because DMEK has rapid visual recovery and the least risk of immunologic rejection, these goals occur over a compressed timeline compared with other forms of keratoplasty. While the steroid tapering strategy will vary between surgery centers, we typically taper over a 12 to 18 month period. Visual recovery is less predictable, and comanaging optometrists should be aware that while DMEK usually provides recovery of vision by three to six months, some eyes won’t fully stabilize for the first year. If vision is not as good as expected, yet the graft appears healthy and the cornea is clear, patience is advised; many of these eyes will continue to improve well beyond the first months.
While DMEK’s surgical complexity and potential for early graft dislocation has slowed its dissemination to some degree, its potential for superior visual outcomes and reduced risk of corneal graft rejection create a place for its use in the treatment of our patients with endothelial disease.
Dr. Bronner is a staff optometrist at the Pacific Cataract and Laser Institute in Kennewick, Wash. He has no financial interest in any products described in this article.
1. Melles GR, Ong TS, Ververs B, van der Wees J. Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2008;145:222-7.2. Price MO, Giebel AW, Fairchild KM, Price FW Jr. Descemet’s membrane endothelial keratoplasty: Prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology. 2009;116:2361-8.
3. Anshu A, Price MO, Price F. Risk of corneal transplant rejection significantly reduced with DMEK. Ophthalmology. 2012;119:536-40.

