Editors note: This month we welcome Dr. Pewitt as our Therapeutic Review columnist. Dr. Pewitt practices with the Veterans Affairs Healthcare System in San Diego.
As comanaging doctors for cataract and refractive surgery, optometrists must be skilled in the use of topical antibiotics to prevent infections, treat those that occur and avoid overtreating. Here, well offer some guidelines for comanaging patients.
Cataract Patients
The incidence of ocular infection following cataract surgery ranges from 0.05% to 0.5%.1 About 85% of bacterial endophthalmitis isolates are Gram-positive, and 15% are Gram-negative.2,3 The most commonly isolated organisms are coagulase-negative Staphylococci (CNS) and Staphylococcus aureus. Less common isolates are Corynebacterium acnes, Micrococcus species, and Gram-negative rods including Pseudomonas aeruginosa.4
The optimal characteristics of antibiotics used for perioperative endophthalmitis prophylaxis include the ability to kill bacteria and broad-spectrum coverage, particularly for Gram-positive bacteria. Common medications used include:
Aminoglycosides. Frequently used aminoglycosides include neomycin, amikacin, gentamicin and tobramycin. Recent studies show that we can effectively treat Gram-positive organisms with neomycin and amikacin, but there are increasing rates of resistance to gentamicin and tobramycin, possibly due to more frequent and widespread use.5
Fluoroquinolones. Second- and third-generation agentsciprofloxacin, norfloxacin and ofloxacinhave good susceptibility patterns against most Gram-positive and negative organisms. An exception: Pseudomonas, which has shown increased resistance to ciprofloxacin.6
The fourth-generation fluoroquinolonesgatifloxacin and moxifloxacinhave susceptibilities similar to the second- and third-generation drugs. In one study, they were more potent than second- and third-generation agents for Gram-positive bacteria and equally potent for Gram-negative bacteria, but showed increased susceptibility in S. aureus isolates that were resistant to the earlier-generation drugs.2
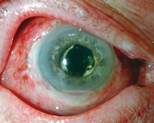
Patient with endophthalmitis exhibits hypopyon. ourtesy: Trey Sullins III, O.D.
Cephalosporins. Cephalothin, a first-generation cephalosporin, is effective in treating CNS, but S. aureus and Pseudomonas have shown increasing resistance to cepalothin.5 There is even a higher rate of S. aureus resistance to the third-generation cephalosporin, ceftazidime, so we do not recommend this agent.7
Chloramphenicol. This broad-spectrum antibiotic has been used to treat various infections.
Refractive Surgery
Post-operative ocular infection after refractive surgery may lead to significantly reduced visual acuity. Infectious keratitis and endophthalmitis are of concern and need quick diagnosis and treatment.
The incidence of infectious keratitis after LASIK is unknown. In one survey, 56 LASIK surgeons reported some 116 infections out of an estimated 338,550 procedures.8
Post-op care of the refractive surgery patient includes a prophylactic antibiotic, a steroid and artificial tears. Often, an antibiotic- steroid such as Tobradex (tobramcycin/dexamethasone, Alcon) is useful. Add a hypertonic saline if theres significant corneal edema and consider a topical NSAID if the patient reports ocular discomfort.
Consider any focal infiltrate after LASIK to be infectious until proven otherwise. The organism is usually acquired intraoperatively and becomes pathogenic only after the antibiotic prophylaxis is discontinued.
The most common organisms associated with post-LASIK infections are Mycobacterium and staphylococci. Infections most often occur within 72 hours of surgery with an acute onset of symptoms.9 Delayed-onset keratitis is commonly due to atypical mycobacteria, fungi, and the Gram-positive Nocardia.
Send the patient back to the surgeon if you suspect postoperative infection. The surgeon will need to lift the flap, scrape for cultures then flush the area with antibiotics. Early diagnosis and treatment of bacterial keratitis is critical for maintaining good visual acuity.
The Right Choice
Gram-positive organisms cause most cases of endophthalmitis and bacterial keratitis, so choose an antibiotic with good Gram-positive coverage. Tobramycin and gentamicin are showing decreased susceptibility to Streptococcus and S. aureus.5 Consider another aminoglycoside, such as neomycin, or a fluoroquinolone.
The development of bacterial resistance to antibiotics remains a major concern. Resistance can emerge through mutation or by horizontal transfer of genes or gene fragments.10 Second- and third-generation fluoroquinolones require one bacterial mutation, but the fourth-generation fluoroquinolones require two mutations to establish resistance.11 So, they provide better coverage against Gram-positive bacteria that are resistant to second- and third-generation drugs.
Appropriate antibiotic use is essential to prevent and control resistance.
Generally, patients should use antibiotics long enough to eradicate the microorganism yet minimize adverse reactions. When in doubt, reduce duration of treatment and do not taper antibiotics.
We must remain well-versed in the use of antibiotics following cataract and refractive surgery. Early diagnosis and treatment of post-op infection is necessary to maintain good visual acuity.
1. Schmitz S, Dick HB, Krummenauer F, Pfeiffer N. Endophthalmitis in cataract surgery: results of a German survey. Ophthalmology 1999 Oct;106(10):1869-77.
2.Mather R, Karenchak LM, Romanowski EG, Kowalski RP. Fourth generation fluoroquinolones: new weapons in the arsenal of ophthalmic antibiotics. Am J Ophthalmol 2002 Apr;133(4):463-6.
3. Donahue SP, Kowalski RP, Eller AW, et al. Empiric treatment of endophthalmitis. Are aminoglycosides necessary? Arch Ophthalmol 1994 Jan;112(1):45-7.
4. Ta CN, Chang RT, Singh K, et al. Antibiotic resistance patterns of ocular bacterial flora: a prospective study of patients undergoing anterior segment surgery. Ophthalmology 2003 Oct;110(10):1946-51.
5. Chalita MR, Hfling-Lima AL, Paranhos A Jr, et al. Shifting trends in in vitro antibiotic susceptibilities for common ocular isolates during a period of 15 years. Am J Ophthalmol 2004 Jan;137(1):43-51.
6.Mutnick AH, Rhomberg PR, Sader HS, Jones RN. Antimicrobial usage and resistance trend relationships from the MYSTIC Programme in North America (1999-2001). J Antimicrob Chemother 2004 Feb;53(2):290-6.
7. Kunimoto DY, Das T, Sharma S, et al. Microbiologic spectrum and susceptibility of isolates: part I. Postoperative Endophthalmitis. Endophthalmitis Research Group. Am J Ophthalmol 1999 Aug; 128(2):240-2.
8. Solomon R, Donnenfeld ED, Azar DT, et al. Infectious keratitis after laser in situ keratomileusis: results of an ASCRS survey. J Cataract Refract Surg 2003 Oct;29(10):2001-6.
9. Pushker N, Dada T, Sony P, et al. Microbial keratitis after laser in situ keratomileusis. J Refract Surg 2002 May-Jun;18(3):280-6.
10. Lipsitch M, Samore MH. Antimicrobial use and antimicrobial resistance: a population perspective. Emerg Infect Dis 2002 Apr;8(4):347-54.
11. Kowalski RP, Dhaliwal DK, Karenchak LM, et al. Gatifloxacin and moxifloxacin: an in vitro susceptibility comparison to levofloxacin, ciprofloxacin, and ofloxacin using bacterial keratitis isolates. Am J Ophthalmol 2003 Sep;136(3):500-5.

