 |
A 51-year-old white female presented to the office as a new patient in May 2005. She reported that she was diagnosed with glaucoma 14 years earlier, with the right eye having suffered more damage than the left, and that her pressures are stable.
Her last visit with her previous eye care provider was six months earlier. She reported that she was interested in transferring her care because our office is closer to her home and work than that of her previous provider. Also, the waiting time at the previous providers office has steadily increased over the past few years. She remarked that she really will miss her previous provider, as they have always gotten along so well.
Diagnostic Data
Current medications include Lumigan (bimatoprost, Allergan) one drop h.s. O.U., Betagan 0.5% (levobunolol, Allergan) one drop b.i.d. O.U., estradiol q.d., Effexor XR (venlafaxine, Wyeth) p.r.n. and vitamins. She reported an allergy to penicillin and Duricef (cefadroxil, Bristol-Myers Squibb). She reported that her mother has had glaucoma for many years and was also diagnosed at a young age.
Prior to her visit to our office, she signed a records release form from the previous provider. A summary letter of her care was sent to me prior to my meeting with her. According to the letter, she was initially diagnosed with glaucoma in 1992 with entering pressures of 30mm Hg O.D. and 27mm Hg O.S., and cup-to-disc ratios of 0.60 x 0.90 O.D. and 0.60 x 0.70 O.S. The letter said she has an extensive Bjerrum scotoma superiorly O.D. and an early Bjerrum scotoma superiorly O.S.
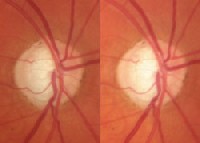 |
| A stereoscopic photo of the right eye shows a thinned neuroretinal rim superiorly and inferiorly. |
At her first visit to our office, uncorrected visual acuity was 20/20- O.U. Pupils were equal, round and reactive to light and accommodation with no afferent pupillary defect. Applanation tensions at 10a.m. were 9mm Hg O.D. and 10mm Hg O.S. Pachymetry readings were 497m O.D. and 499m O.S. Slit lamp examination of her anterior segments was unremarkable except for minimal inferior corneal stippling.
Through dilated pupils, her crystalline lenses were clear O.U. Stereoscopic examination of her optic nerves demonstrated C/D ratios of 0.85 x 0.95 O.D. and 0.80 x 0.80 O.S. The neuroretinal rims were thinned superiorly and inferiorly O.U., with marked notching of the right rim at 6 oclock. Stereoscopic disc images were obtained as baseline records. The macular and peripheral retinal examinations were unremarkable. Visual fields and gonioscopy were not performed at this initial visit.
 |
|
Visual fields demonstrated a dense superior arcuate scotoma, O.D. |
She immediately asked, Why so soon? My previous doctor only saw me every six months for years, and I have always been stable. I dont need to be seen so soon.
I knew instantly that I was dealing with a patient who had become accustomed to visits at six-month intervals. Since this was her first visit and we didnt have time to establish a good doctor/patient relationship, I explained the reason for the three-month follow-up this way: Due to time constraints at our first visit, we did not complete all of the testing necessary to establish baseline information, and in the interest of time we would complete those at the next visit three months down the road.
The patient agreed to return in three months to complete the evaluation.
Discussion
I knew that I was putting off an inevitable discussion with the patient, but in the interest of not parting ways on the initial visit with a negative feeling, I thought it would be best to have that discussion when (and if) she returned at the three-month interval. Of course, the discussion to be had was the one dealing with the necessity of more frequent visits to monitor her optic nerves, and an explanation as to why this more frequent schedule was ultimately in her best interest.
Somewhat surprisingly, the patient did return to the office in August 2005 for fields, gonioscopy, tensions and a nerve evaluation. At that visit, applanation tensions were 10mm Hg O.D. and 11mm Hg O.S. Gonioscopy demonstrated grade III+ open angles O.U. with minimal to trace trabecular pigmentation. Visual fields demonstrated a dense superior arcuate scotoma O.D. involving fixation and a superior arcuate depression O.S. Her nerves were as described at the last visit. Convinced that the patient was in fact relatively stable, I made no changes to her current medication regimen.
At the completion of the physical examination, I began a frank discussion with the patient regarding the severity of her glaucomatous optic nerve damage, the fact that she was young and, most importantly, that her previous track record of stable IOP, nerves and fields was no guarantee that they would remain stable. In fact, I said, As you get older, your likelihood of remaining stable diminishes.
She knew exactly where I was going with the discussion and said she did not feel it was necessary to be seen more often than twice a year.
I am sure you have seen patients like this. How would you proceed?
Management
As I looked at the situation over the next several days, I found I had three options:
Lay down the law. I could explain to the patient that glaucoma is a serious condition and requires therapy and monitoring according to the schedule I set, independent (within reason) of what the patient thinks is reasonable. This is relatively easy with a patient with whom you have already established a relationship, but it is more difficult with a new patient. The risk: The patient may decide to leave and return to the original provider. Is that really in the patients best interest: to return to a provider who believes that minimal monitoring of a young patient with advanced disease is appropriate?
Please the patient. The opposite option: See the patient on her preferred schedule. You wont risk losing the patient, but is this option really in her best interest?
Compromise. Perhaps some agreement could be worked out with the patient whereby she is evaluated more frequently than she is accustomed to, but somewhat less frequently than I would like.
Sure, were used to negotiating with a patient who is unhappy with her eyewear. But negotiating over her care? Were doctors, and negotiation over care is a difficult concept. But negotiating with patients such as this one can result in a win/win situation. So, we must be prepared to adapt our office protocols accordingly, without ever compromising care. And that can be a hard thing to do.
One way to help in this regard is to remember this mantra: Keep the patients best interest at heart at all times. In this case, I truly did not believe it was in her best interest to return to her previous provider. Her disease is simply too advanced, and she is too young to be seen at the schedule to which she is accustomed. Nor was it in her best interest to let her call the shots on the frequency of visits. What was in her best interest was to continue her care with me in a way that was also comfortable for her.
So I negotiated with her. Instead of twice a year, she agreed to be seen three times a year. Its not quite the quarterly visit schedule I feel most comfortable with, but it will suffice for now. My goal, however, is to develop a good, trusting relationship with her and to gradually insinuate a change in her follow-up schedule, assuming everything remains stable.
But the instant that her condition becomes unstable, there will be little room for negotiation.

