 |
| Though scleral lenses can temporarily flatten corneas, it only takes one overnight for changes to revert to baseline. Photo: Mitch Ibach, OD. Click photo to enlarge. |
Though there is no physical interaction between a scleral lens and the wearer’s cornea, studies have observed transient corneal curvature and thickness changes in both healthy and keratoconic eyes with scleral lens use. These changes could potentially be caused by several things; curvature changes may be attributed to positive or negative fluid pressure, stress surrounding the limbus or corneal edema, and corneal thickness could occur due to lens thickness, a thicker post-lens tear film layer or the absence of lid wiper chafing while blinking during lens wear.
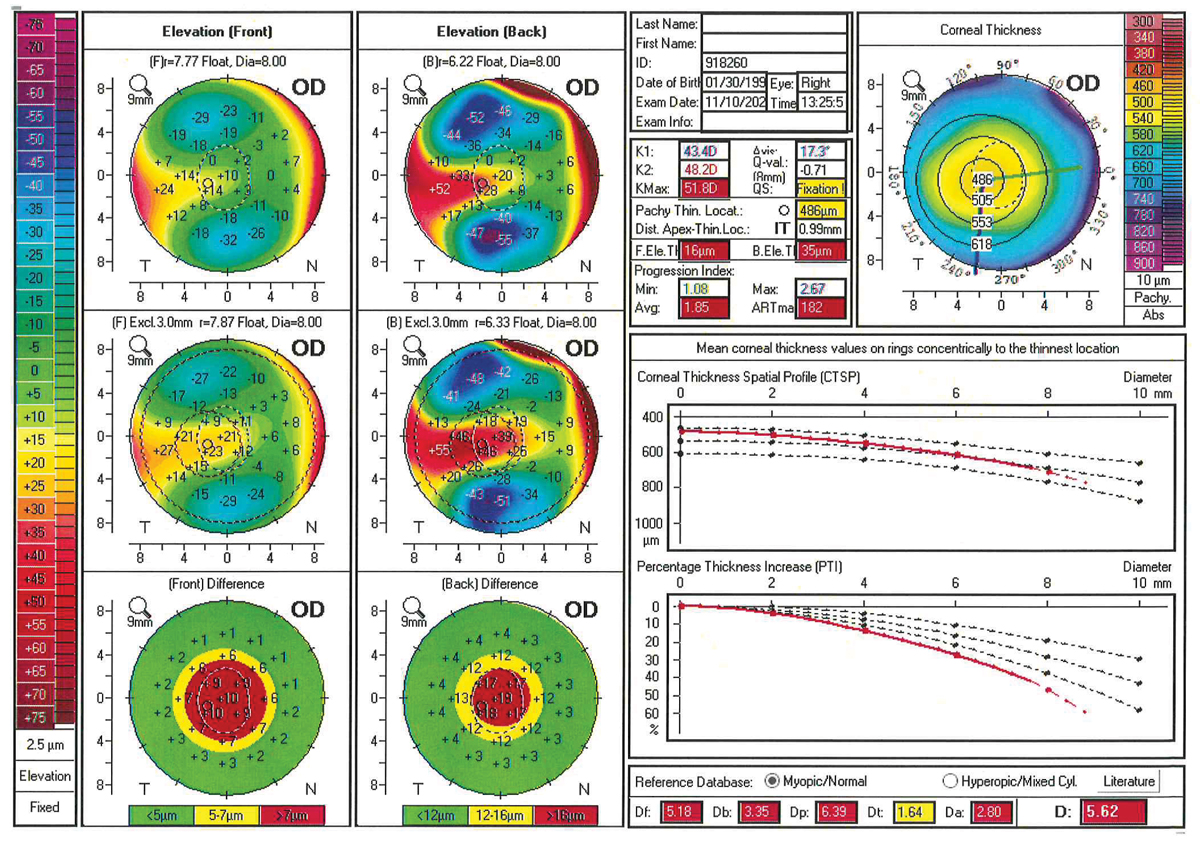
In keratoconus patients who wear scleral lenses, these temporary changes make it more difficult to monitor disease progression and determine the best treatment option, hence why patients are asked to discontinue lens wear prior to topography measurement. While the necessary duration of discontinuation for ensuring accurate test results has not yet been defined, researchers recently investigated the recovery period of these temporary changes. After six hours of lens wear in keratoconic patients, they observed minimal transient alteration in the anterior corneal curvature and corneal thickness, which regressed to baseline the following morning after one night of lens removal.
The study included 17 eyes of 12 patients with keratoconus. Scheimpflug imaging was captured at the following intervals: before lens insertion, six hours after lens removal and the next morning. Anterior flat, steep and maximum keratometry (Kflat, Ksteep and Kmax, respectively) and pachymetry values were compared.
“The average Kflat was 0.28D flatter, Ksteep was 0.37D flatter and Kmax was 0.19D flatter, which returned to baseline level after one night of lens removal,” the researchers wrote in their paper. “The mean corneal clearance after five minutes of lens insertion was 448mm, and final central corneal clearance after six hours of lens wear was 368mm. The mean reduction in central corneal clearance after six hours of lens wear was 80mm. There was no significant relationship found between reduction in central corneal clearance and the change in central corneal thickness.”
Although a larger study may help expand these findings, the results conclude that short-term scleral lens wear does induce a minimal amount of flattening in the anterior corneal curvature parameters and corneal edema. The researchers suggest advising keratoconus patients to discontinue scleral lens wear for at least one night to allow these changes to regress back to baseline prior to performing corneal topography measurements.
Iqbal A, Mahadevan R. Impact of scleral lens on corneal curvature and pachymetry in keratoconic eyes. Cornea. July 21, 2021. [Epub ahead of print]. |


