A 58–year–old female presented with a chief complaint of a swollen eye. The patient also said that she perceived what seemed like "a significant number of gnats" in her vision. She had been working in the garden the previous evening before the symptoms began. The patient had a refraction of roughly –6.50 OU. She noted that her symptoms largely were isolated to her right eye, and—to make matters worse—she also developed a rash on her face, close to her right eye, that appeared to be caused by exposure to poison ivy. The patient was prescribed topical hydro-cortisone ointment for the rash and returned home.
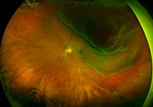
Two days later, the patient called the office to report an area of missing vision in the lower right quadrant of her right eye. She was scheduled for an appointment later that day. Unfortunately, after being examined a second time and referred to a local ophthalmologist for the follow-ing day, the patient experienced a macula–off retinal detachment later on that evening.
Malpractice cases often involve the chaining together of numerous clinician errors and over-sights. In this case, these included the "red herring" secondary to the poison ivy rash; not evaluating for the presence of floaters for three days in a relatively high myope; and failing to promptly refer the patient for an ophthalmology consult on the same day as the patient’s return visit, when she complained of missing vision.
Pearls we can garner from this case:
- Patients who complain of new floaters (either one large floater or many floaters)—with or without flashes, even if not the primary complaint—require dilation and a thorough fundus examination.
- Although any patient can experience a retinal detachment, think of this possibility in highly myopic patients—especially in situations where symptoms present while the patient was bending over, such as while gardening.
- When a field of vision is missing, remember to spend additional time examining the contralateral field or inverted retinal area. In this case, for example, an inferior or lower-right quadrant requires an extensive examination of that eye’s superior nasal quadrant. Examine the entire retina first, and then go back and look at that specific quadrant one more time in greater detail.
- Look for pigment in the vitreous (often referred to as "tobacco dust"). This presentation is a telltale indication of a retinal detachment. This situation warrants prompt referral, even if you are unable to locate a tear or detachment.
|
 |





![]()