| |
|
| Vol. 1, #13 • Thursday, December 10, 2020 |
|
|
|
|
| |
|
Review's Chief Clinical Editor
Paul M. Karpecki, OD, FAAO
Provides you with cutting-edge clinical strategies for optimal management of ocular surface disease and beyond.
|
|
|
|
|
|
 |
| A microbial keratitis should initially be treated with antibiotics only and cycloplegia for pain. |
|
-
Although topical corticosteroids are essential to the management of ocular surface diseases including dry eye disease (DED), understanding when to avoid corticosteroids is the focus of today’s clinical pearl.
Topical steroids are absolutely necessary in effective clinical management of patients experiencing inflammatory eye disease, so avoiding them is not the intent of this clinical pearl. In fact neglecting to use topical steroids in cases where they are indicated can lead to permanent scaring, irregular healing, distortion or irregularity of the cornea, and even the risk of adaptive immunology development and chronic disease. However, as with any therapy, you want to apply topical corticosteroids in cases that justify their use.
Here is a guide to potential contraindications for use of ocular corticosteroids.
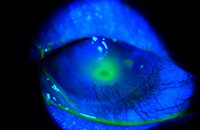
1. If a potential infectious keratitis is present, avoid the use of topical corticosteroids including combination agents, as many studies are inconclusive about their benefits in such cases, with some findings, like epithelial herpetic keratitis, showing worse outcomes. In general, microbial keratitis is accompanied by significantly more pain, photophobia, discharge, redness (often 360 degrees), and vision loss. The infiltrate tends to be more central, and an anterior chamber reaction is often present. The abrasion over the infiltrate tends to be larger or at least close to the size of the infiltrate in microbial keratitis, and infectious corneal ulcers typically develop acutely. If there is any doubt about the findings, it’s best to begin with an antibiotic alone and have the patient return the next day. If the ulcer turns out to be sterile, then adding a steroid combination agent the next day won’t affect the outcome, but it’s impossible to remove a steroid that’s already been applied.
2. The first time you write a prescription for a topical corticosteroid, consider writing zero refills. Steroids work exceptionally well and suppress inflammation better than any agent we have at our disposal. For this reason, most patients will improve dramatically, and they may cancel a follow-up appointment because their eyes feel so comfortable. Multiple refills could mean long-term use of a topical corticosteroid without the opportunity to measure intraocular pressure (IOP). If the patient tends to have periodic flareups, consider the option of refills in subsequent visits, once you ascertain the patient is not a steroid responder, and is responsible with their drops and follow-up visits.
3. Don’t use topical corticosteroids on corneal abrasions. The majority of abrasions don’t warrant the use of topical corticosteroids and may even slow down healing. In the case of an abrasion, it’s best to prescribe a topical antibiotic and bandage contact lens. If pain is significant, assess the possibility of cycloplegia, and consider the use of topical or oral NSAIDs rather than a corticosteroid. If a persistent epithelial defect (PED) is the issue, consider amniotic membrane or treating the neurotrophic keratitis that may be causing the defect while maintaining antibiotic prophylaxis.
4. In patients with poorly controlled autoimmune diseases such as rheumatoid arthritis or diabetes, avoid using topical corticosteroids. This is not an absolute contraindication, but if the patient’s disease is not well-controlled or being managed by a specialist, don’t prescribing a steroid until systemic disease control is achieved or more frequent follow-up visits are required.
5. Don’t apply topical corticosteroids over a contact lens. Contact lenses can serve as depots for medications and increase contact time with the eye. This in turn can lead to elevated IOP, or because of local immune suppression, the development of microbial keratitis.
6. Glaucoma patients and children have a higher incidence of IOP rise with the use of corticosteroids. In these cases, consider all other possible therapeutic agents to control inflammation. If steroids are still indicated, consider short-term therapy and monitor more closely.
Knowing these insights should enhance your confidence in prescribing topical corticosteroids in appropriate inflammatory eye disease management.
|
|
|
|
KEY TAKEAWAY: The key to effective use of topical corticosteroid in management of ocular surface disease is understanding when steroids are and are not indicated.
|
|
|
|
| Supported by an independent medical grant from Kala Pharmaceuticals |
|
| |
| |
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 19 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|
|
|
|
|
|
|
|