 |
|
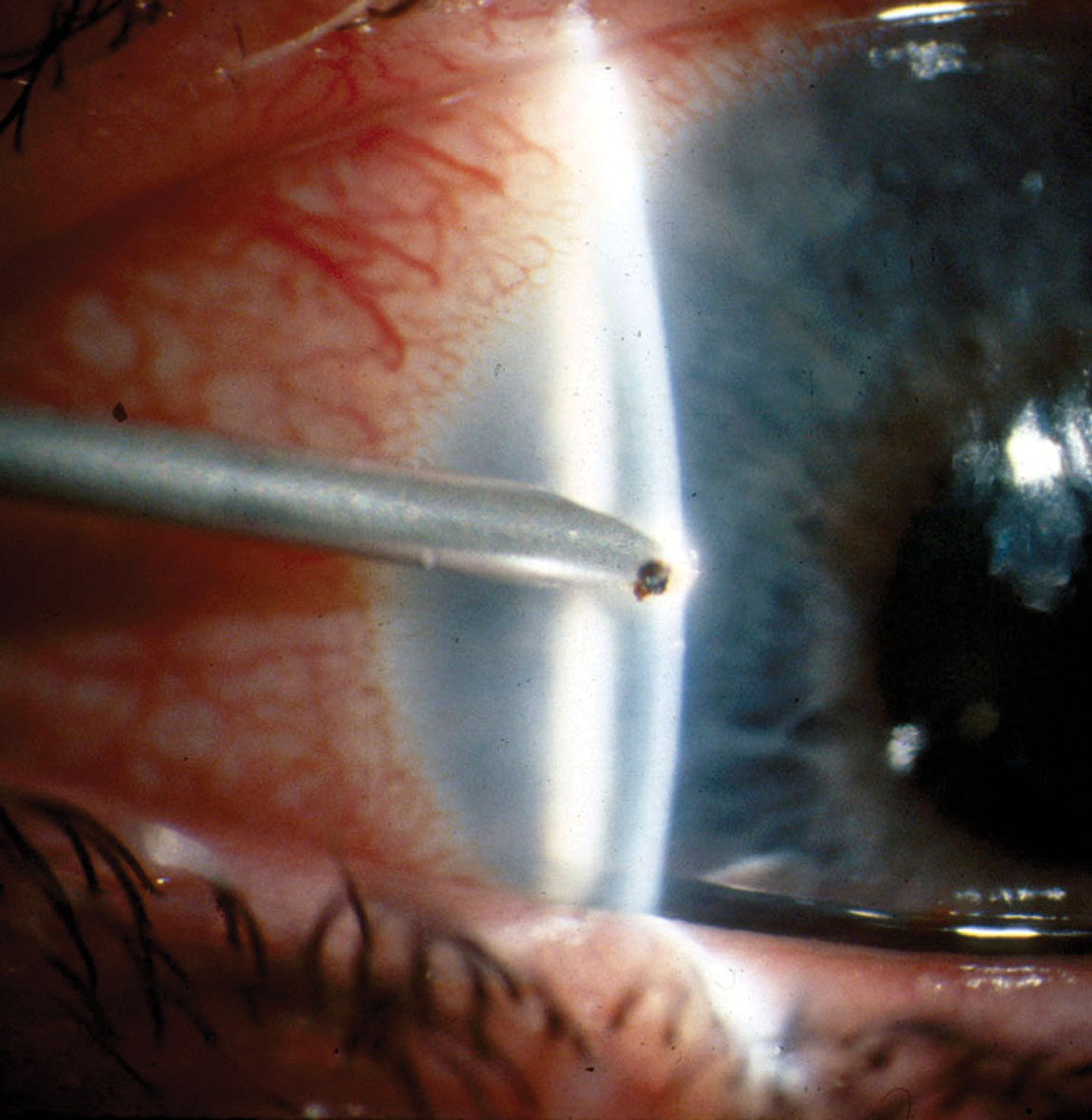
The incidence rate of infectious keratitis within three days post-corneal foreign body removal was around 5% in this study and non-dependent on treatment (antiseptics vs. antibiotics). Photo: Bridget C. Hendricks, OD. Click image to enlarge. |
Clinicians need to be mindful of infection risk in patients with a corneal foreign body, given the potentially devastating effects on vision. As a result of contaminants exposed to the ocular surface during removal, infectious keratitis is a common complication, which ultimately leads to visual impairment in nearly 3% of cases. Optometrists and ophthalmologists alike typically prescribe antibiotics post-removal to mitigate the risk of infection, even though few studies have evaluated the effectiveness of this protocol. To gain some clarity on preferred techniques, a recent study evaluated the performance of two treatments—antibiotics and antiseptics—on foreign body removal outcomes. It also sought to compare outcomes of burr vs. needle removal. The findings, published in the journal Eye, suggested the two drugs have a similar effect; however, the authors reported that using a burr instead of a needle for the removal procedure was associated with longer healing time.
The retrospective study involved a predominantly male cohort (300 of 307) with a mean age of 43, all of whom were referred for corneal foreign body removal (95.1% were metallic, and rust was found in 72.1%). Patients were treated with either picloxydine (group 1; n=155) or tobramycin (group 2; n=152). About half were building workers (50.2%), and the majority (68.1%) weren’t wearing protective eye gear when the injury occurred. To remove the foreign body, a burr was used in 38.9% of cases.
Roughly 5% of patients developed infectious keratitis following removal (5.3% in group 1 and 4.5% in group 2), which was successfully resolved in all cases with a combination of two antibiotics. Persistent rust was present in 36.9% of patients on day three, and its incidence appeared to be unaffected by procedure method (burr vs. needle).
Also on day three post-removal, corneal scars were present in 57.4% of patients. The researchers reported in their paper, “The corneal foreign body size, the use of a burr and the presence of rust after removal were not associated with corneal scarring. In the multivariate analysis, only non-iron corneal foreign bodies were significantly associated with the presence of a corneal scar on day three.”
Corneal ulcers persisted in 47.2% of patients on day three, mainly in the burr-treated group. The multivariate analysis concluded that “the mean time to consultation, presence of rust on day zero and use of a burr for corneal foreign body removal were significantly associated with the persistence of a corneal ulcer on day three.”
While the researchers found that the use of antibiotics vs. antiseptics didn’t affect short-term outcomes of corneal foreign body removal, they noted that “compared with traditional needles, the use of a burr did not remove the rust better and was associated with a corneal healing delay at day three.”
Rebattu B, Baillif S, Ferrete T. Corneal foreign bodies: are antiseptics and antibiotics equally effective? Eye. January 13, 2023. [Epub ahead of print]. |


