 |
|
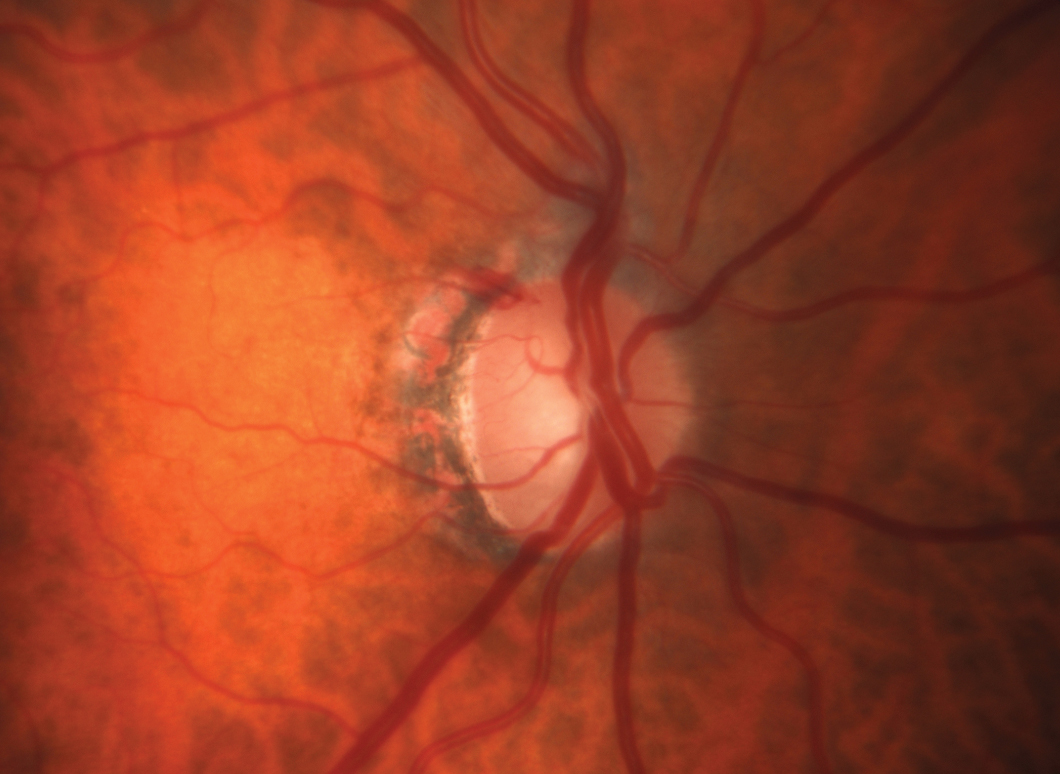
The apolipoprotein E4 allele variant was observed to have an inverse relationship with glaucoma but was also associated with increased dementia. Photo: Michael Chaglasian, OD, and Sarah B. Klein, OD. Click image to enlarge. |
The increasing sophistication of genome-wide association studies creates optimism that specific mutations can be identified that might enable genetic screening to reveal individuals vulnerable to glaucoma prior to disease onset. But a new analysis of a large dataset found the connections to be more complex and less predictive than previously supposed. Apolipoprotein E (APOE), in particular, the E4 subvariant allele, was observed in relation to cases of glaucoma.
The researchers used the UK Biobank (UKBB) to gather information and included those who were genetically determined to be of European ancestry. This was to mitigate any potential confounding resulting from ethnicity, which has been established to be an important covariate of glaucoma and E4 allele presence. A total of 438,711 people were included.
In addition to using data from this set, replication analyses were performed (using clinical and genotyping data) from the sets of the Canadian Longitudinal Study of Aging (18,199 European participants), the Australian and New Zealand Registry of Advanced Glaucoma (1,970) and the Blue Mountains Eye Study (2,440).
When determining correlations, the researchers decided to look at distribution of APOE alleles and genotypes. These were then compared on glaucoma status basis, and other analyses were performed in a similar fashion. This was done using positive control outcomes associated with the APOE E4 allele, including death, dementia, and AMD and negative control outcomes not associated with the allele, including cataract and diabetic eye disease. The E4 allele was also associated with the clinical outcome of Alzheimer’s dementia (AD), an outcome phenotype.
What they found was an inverse relationship of the APOE E4 allele and glaucoma, as well as the allele with both negative controls in the UKBB database. There was an opposing, positive correlation between AD and glaucoma as well as cataract. Even further, the E4 allele displayed no association with glaucoma in either of the replication data sets.
The researchers of the study infer that the small, negative correlation seen in the UKBB dataset might represent “an artifact of glaucoma underdiagnosis in APOE E4 carriers.” This is to say that the researchers essentially believe the observed association to be resultant of inherent study biases rather than actual neuroprotection of the allele.
They add that glaucoma prevalence of the UKBB (3.2%) was lower than the estimated prevalence for Europeans, with the lowest estimate being at 6.0% for those aged 60 to 69 years old. Low rates also appeared in the CLSA (5.0%) and BMES subsets (5.2%), potentially being consequential of under-reporting of glaucoma from the data collection methods used.
A similarly low rate of AD was reported in the UKBB at 0.4%, sticking out as an outlier from the estimated prevalence to be of 6.8% for Western Europeans greater than 60 years of age. This could possibly be due to underdiagnosis and under-reporting, since the study follow-up was long. Despite this fact, the study points to confounding from dementia-associated executive dysfunction with observed E4 allele depletion characterized by pathophysiologically unrelated phenotypes.
To summarize what this may mean going forward, the authors of the study agree that “although the E4 allele may contribute to glaucomatous neurodegenerative consequences, this study highlights the complicated interactions between an allele associated with increased dementia and mortality risk and underdiagnosed ocular phenotypes.”
Mullany S, Diaz-Torres S, Schmidt JM, et al. No strong association between the apolipoprotein E E4 allele and glaucoma: a multicohort study. Ophthalmol Sci. 2023. [Epub ahead of print]. |


